Most Common Cause of Vaginitis
Most women experience itching, discomfort, swelling, an unusual discharge, and pain down there at some point. These often indicate vaginitis. The most common cause of vaginitis is bacterial infection, but yeast infection and certain sexually transmitted infections can also be the culprits. If you notice the above symptoms and feel any unusual change in your vaginal health, visit an obstetrician-gynecologist in Navi Mumbai to diagnose the underlying cause. In the meantime,
let’s explore the most common cause of vaginitis.
i) Bacterial Vaginosis
There’s usually a mix of good and bad bacteria, with good bacteria keeping the vaginal environment slightly acidic. Bacterial Vaginosis (BV) occurs when there’s an increased amount of bad bacteria in your vagina.
a) BV Causes:
BV can be linked to douching and using scented products, which can affect the pH balance of your vagina. It’s also more common in women with multiple sexual partners, as it increases the risk of bacteria entering your vagina.
b) BV Symptoms:
If there’s an overgrowth of the bad bacteria, you might develop bacterial vaginosis, causing grayish discharge, a fishy odor, vaginal itching, and discomfort.
c) BV Treatment:
Treatment includes an antibiotic course. Make sure you take the pills even if the symptoms improve, as there’s a risk of recurrence.
ii) Yeast Infections
The overgrowth of Candida albicans — a fungus that naturally thrives in your vagina — can cause vaginitis. It’s also found in other moist areas of your body and is also a common reason for diaper rash in babies.
d) Yeast Infection Causes:
Yeast infection occurs because of hormonal changes and increased blood glucose levels in people who are taking antibiotics. Antibiotics kill good bacteria, which are responsible for keeping Candida albicans in check.
e) Yeast Infection Symptoms:
Symptoms include itching and redness around the vulva with thick discharge.
f) Yeast Infection Treatment:
Antifungal creams and oral medication can help clear yeast infections. You can also take probiotic supplements to restore a healthy balance of good and bad bacteria. Lifestyle changes, like avoiding damp and tight clothing, can also help.
iii) Trichomoniasis
Trichomonas vaginalis is transmitted through sexual intercourse with an infected partner. The infection affects the urinary tract system in men and the vagina in women.
g) Trichomoniasis Symptoms:
Symptoms may vary from woman to woman, but most infected people experience itching, greenish-yellow discharge, and pain during urination and intercourse.
h) Trichomoniasis Treatment:
Oral antibiotics can help clear Trichomoniasis. Avoid sexual activity until it’s completely cleared.
iv) Other Less Common Causes
Vaginitis is also linked to causes other than bacteria, parasitic, and fungal infections. Let’s discuss a few less common yet possible causes:
i) Allergic Reaction:
Scented products, such as soaps and creams, can cause an allergic reaction or may simply irritate your vagina, causing a burning sensation and redness. The sensitive skin of your vagina can also become swollen and red from the laundry detergents and condoms.
j) Vaginal Atrophy:
Women approaching menopause or post-menopausal women are at increased risk of vaginal atrophy due to a decreased production of estrogen. Your vaginal walls become thin and dry without estrogen, increasing the risk of vaginitis. Your gynecologist will run tests to diagnose the cause and offer the most appropriate vaginitis treatment in Navi Mumbai. See your doctor if you notice the above symptoms. Stay healthy!!

How to Stop Diarrhea in Infants?
Baby’s poop can be of different colors, textures, and odors, depending on their age and what they are eating (breastmilk, formula, or solids). It’s usually softer than an adult’s poop and can vary in frequency. However, if you notice stools that are too watery, loose, and more frequent than usual (three or more) in 24 hours, it could indicate diarrhea. Let’s check out the causes, symptoms, and treatment for pediatric diarrhea in Navi Mumbai.
Common Causes of Diarrhea in Infants
Here’s what may cause diarrhea in infants:
a) Viral Infections:
A viral infection is the most common cause of diarrhea in babies. Rotavirus and other viruses can spread easily by touching contaminated surfaces. Fortunately, vaccines are available for viral infections.
b) Bacterial Infections:
E. coli, Salmonella, and Shigella are common bacteria that can cause diarrhea with fever, stomach cramps, and vomiting in infants. Some are found in undercooked foods, and others may spread in certain environments, like daycare.
c) Food Allergies:
Your baby could be lactose intolerant or have a cow’s milk protein allergy. If they consume these foods or the breastfeeding mother consumes lactose-rich products, the baby could experience diarrhea.
d) Teething:
When infants start teething, they develop the habit of chewing on nearly everything they get. This can introduce germs to their mouth, leading to episodes of diarrhea. Teething also leads to excessive saliva production, which, when swallowed, can cause loose stools.
Recognizing Symptoms of Diarrhea
The most common symptom of diarrhea in infants is dehydration. It can happen pretty quickly (within 2-3 days or sooner) if the baby consistently passes loose, watery stools. Depending on the cause of the diarrhea, the parents might notice other symptoms, such as:
- Blood in the stools
- Vomiting
- Fever
- Abdominal pain
How to Stop Diarrhea in Infants? Home Remedies and Care Tips
Immediate care and medical attention (in severe cases) are required. However, these tips are often effective for mild diarrhea:
i) Adequate Hydration:
Continue offering breastmilk and formula to your baby to keep them hydrated. Breastfeeding provides many essential nutrients and antibodies that help your baby recover quickly. If required, you can offer a few sips of ORS to maintain the electrolyte balance and restore the lost fluid.
ii) Appropriate Dietary Adjustments:
Diarrhea can be a problem in babies who have just started solids. Adjust their diets by focusing more on applesauce, bananas, toast, and rice, which are lightweight on their digestive system. Avoid fruit juices and other sugary foods until their digestive health improves.
iii) Importance of Hygiene:
Diarrhea can lead to frequent diaper changes, which can cause a diaper rash. To avoid that, keep your baby’s genitals clean and dry. Give them diaper-free time.
When to See a Doctor
Mild diarrhea resolves on its own with time. However, if things get out of control and you notice excessively watery stools multiple times a day, it’s best to see a pediatrician in Navi Mumbai. Dehydration is a common complication of diarrhea and can be life-threatening if left untreated. So, take care of your baby’s hydration and maintain good hygiene at home.

What Causes Lower Abdominal Pain in Females?
Cramping or lower abdominal pain is not uncommon in women. When you reach puberty and menstruation begins, you are likely to have dull or sharp pain in the lower abdomen — the area between your belly button and groin. It’s also referred to as pelvic pain. Lower abdominal pain in women can indicate many issues.
Some are normal and just a part of your menstrual and ovulation cycle. There’s a possibility that pelvic can be due to a serious underlying condition, especially if it’s persistent and is accompanied by other unusual symptoms. It’s best to see a gynecologist in Navi Mumbai to rule out any life-threatening condition. Let’s check out some common causes of pelvic or lower abdominal pain in females.
Menstrual Cramps
Menstruation is the most common cause of pelvic pain in women. It may feel like sharp pain in your upper and lower abdomen and can even spread to the lower back in some cases. The pain is manageable with over-the-counter painkillers and a hot water pad. Menstrual cramps begin before your period starts, as your uterus starts contracting. It can last 2-3 days.
Ovulation Pain
The German word ‘mittelschmerz’ is used to define painful ovulation. In the middle of your menstrual cycle, your ovary releases an egg and fluid. The egg goes down your fallopian tubes into the uterus. The fluid can sometimes enter your abdomen, which may cause irritation and pain. Ovulation pain is temporary and occurs on one side of the pelvis.
Urinary Tract Infections (UTIs)
Lower abdominal pain with painful urination can indicate UTI. Urinary tract infections occur when bacteria from the vagina, skin, or rectal area travel up the urethra into the bladder and occasionally reach the kidneys. UTI can occur in any part of the women’s urinary tract.
Gastrointestinal Issues
Lower abdominal pain could simply be the wind trapped in your abdomen or a sign of constipation. Irritable Bowel Syndrome (IBS) can also cause pelvic pain. If the pain persists and is accompanied by constipation, diarrhea, and other symptoms, it’s advisable to discuss abdominal pain treatment in Navi Mumbai with a certified physician.
Reproductive Health Concerns
Pelvic pain can indicate reproductive health concerns in women. Examples include endometriosis — a condition in which the tissue similar to your uterine lining grows outside the uterus and shed during your period. This can cause excessive bleeding with chronic pelvic pain.
Pelvic Inflammatory Disease (PID) is an infection in the reproductive organs from an untreated sexually transmitted disease. Lower abdominal pain with fever and unusual vaginal discharge are the common symptoms of PID.
Both medical issues can affect your fertility.
When to See a Doctor
- Sharp pain in the lower right abdomen that gets worse over time. It can indicate appendicitis, which can be a medical emergency.
- Persistent pain with fever, chills, and heavy bleeding.
- You suspect an infection that could be causing the pain.
Pelvic pain isn’t always severe or requires a visit to a gynecologist. However, if you notice the above symptoms, seek immediate medical care.
What are the 4 Types of Dialysis?
When your kidneys’ function drops to 10-15 percent, you will be put on dialysis to prevent the accumulation of waste products in your blood. Dialysis imitates the function of your kidneys by filtering excess salt and waste from your blood. Dialysis centers in Navi Mumbai can execute the procedure in four different ways.
If you are wondering what are the 4 types of dialysis, read on.
1) Hemodialysis
Hemodialysis involves a dialyzer, often referred to as an artificial kidney. A machine removes the blood from your body, purifies it through the dialyzer, and transfers the filtered blood back to your body. The procedure lasts between 3 and 5 hours and is needed thrice a week. AV fistula or AV graft can be used to access your blood vessels. Sometimes, the catheter is placed on your neck or chest for quick access.
Pros
- It’s done under medical supervision and is a safe procedure
- Removes all kinds of toxins from your blood efficiently
Cons
- Multiple visits to the dialysis center
- Time-consuming
- Side effects include nausea and dizziness due to low blood pressure
2) Peritoneal Dialysis
If you want flexible dialysis that can be done at home, work, or while you’re asleep, peritoneal dialysis is your safest bet. The kidney dialysis treatment doctor in Navi Mumbai performs a small surgery to insert a catheter into your abdomen, through which dialysate (a special solution) flows into your belly. The peritoneum acts as the natural filter. It collects all toxins from your bloodstream into the solution, which is then drained out.
It’s categorized into two types:
- Continuous Ambulatory Peritoneal Dialysis (CAPD): It’s needed 4-5 times a day while you are awake. Each session takes 30-40 minutes.
- Automated Peritoneal Dialysis (APD): As the name suggests, the dialysis is executed automatically, mostly overnight.
Although it’s the best choice for those who can’t visit the hospital for dialysis frequently or spend 3-4 hours in each session, peritoneal dialysis requires proper incision care. The common risks include infection (peritonitis), weakened abdominal muscles, and hernia.
3) Continuous Renal Replacement Therapy (CRRT)
CRRT is reserved for patients diagnosed with acute kidney failure and those who are monitored in the Intensive Care Unit. Unlike typical dialysis procedures, which last 3-4 hours, this one runs slowly and filters the waste from your bloodstream in a 24-hour cycle. It mimics your kidney function, puts less strain on your heart, and stabilizes your blood pressure. The therapy is the safest choice for critically ill patients whose bodies cannot tolerate regular dialysis.
4) Home Hemodialysis
It’s similar to regular hemodialysis, except you can do it at home. The machine filters your blood and returns the purified blood to your body. The best part about home hemodialysis is that it offers flexibility in running the dialysis machine. You can choose the normal or shorter session that lasts 2-3 hours but is required 5-6 days a week. Nocturnal HHD is another great choice for patients who want a gentle treatment that lasts 5-6 hours and can be executed overnight.
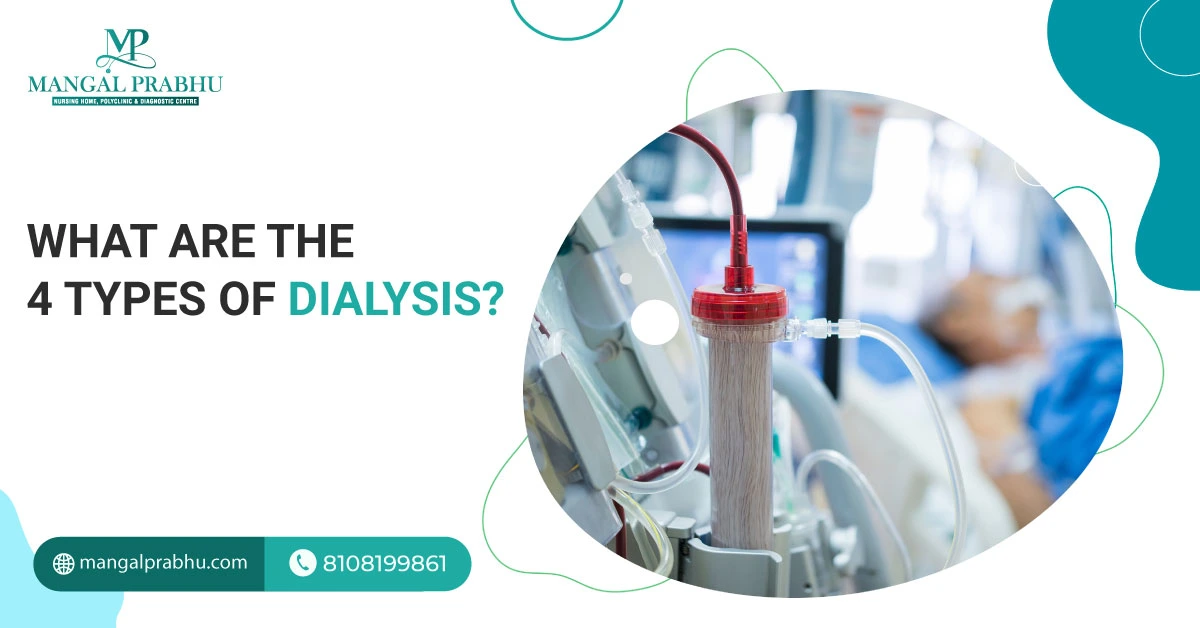
How to Know If ACL Surgery Was Successful?
ACL, short for Anterior Cruciate Ligament, can tear from sudden twisting or turning motion. It’s most likely to happen in athletes, school-goers, and those frequently practicing high-intensity workout sessions and physical activities. Unlike other ligaments, ACL can’t regenerate itself. In fact, in some cases, it doesn’t heal without surgical intervention.
If the tear is too severe, you may need to consult an orthopedic surgeon in Navi Mumbai for potential treatment options. If you have undergone surgical repair, here’s how to know if ACL surgery was successful.
Early Post-Surgery Indicators
Your therapist will set recovery milestones and a timeframe for each. For instance, you should be able to walk without support within a few weeks of surgery and carry out your routine tasks, including physical activity, by 3-4 months. That said, each patient is unique, and so is their recovery period. It’s possible that you can’t walk soon after surgery, but that doesn’t mean your ACL repair surgery has failed. Here are a few early post-surgical indicators of a successful ACL surgery.
i) Reduced Pain
Some pain after ACL surgery is normal. Your surgeon will prescribe medication to relieve post-operative pain. Pain and swelling should resolve in a few days. You can use the RICE (rest, ice, compression, and elevation) to get relief from swelling. If the pain persists or the swelling gets worse after surgery, it might be a sign of graft failure or an infection.
ii) You Can Walk and Move
Another sign of post-operative recovery is the restored range of motion. You will be able to utilize your knee joints like earlier, although the recovery timeline can vary from patient to patient. Mostly, patients are able to straighten their knee joints by week three and bend them after physiotherapy. You can practice quad sets and heel slides to speed up your recovery and restore your full range of motion.
iii) Back To Your Normal Life
Long-term recovery can take time, but you should be able to move your knee joint and perform most activities by the time you hit the 3-month mark. You can gradually start sports within 6-9 months. One of the crucial signs of a successful ACL repair is the absence of instability.
Your knee will feel stable, and you can walk, climb stairs, and execute your routine tasks without collapsing. If you don’t see any improvement in your knee stability and range of motion, it may indicate graft failure. This may require reassessment and revision surgery.
iv) Follow-up Appointments and Imaging
Your surgeon will schedule follow-up appointments to ensure proper and quick healing. They will carefully evaluate your knee stability, movements, and surgical site to rule out postoperative complications.
After ACL surgery in Navi Mumbai, you can have relief from the pain due to arthritis, knee injury, or torn ligaments. If the new graft is precisely implanted and is fully functional, you will see the results within weeks. Improved mobility, reduced pain, minimal to no swelling, and the ability to straighten, bend, and move your knee in all directions are indicators of a successful ACL repair surgery.

Exercises To Avoid After Hernia Surgery
Hernia surgery in Navi Mumbai is an invasive medical procedure that involves pushing the bulging tissue back into its original place. The surgeon might use mesh to strengthen the abdominal muscles and keep the repaired tissue in place. If you have just had hernia repair surgery, you might wonder how soon you can start exercising. We’ve listed some exercises to avoid after hernia surgery and some alternatives you can try.
Understanding Hernia Surgery Recovery
It’s a fairly safe procedure, but like any surgical treatment, hernia repair involves incisions and stitches that can take time to heal. Most patients return to their normal activities in a week or two, but if your work is physically demanding, it’s ideal to wait a little longer or until your doctor clears you for it. It’s not uncommon to feel pain post-operation, accompanied by fatigue and discomfort. The symptoms should resolve within days.
Exercises to Avoid
1) High-impact Activities:
You can start with mild exercises, like walking, but anything that puts strain on the surgical site should be avoided for at least 2 weeks. Running, jumping, aerobics, and all kinds of high-intensity physical activities are a big no.
2) Heavy Lifting or Weight Training:
For a few weeks after surgery, do not lift anything heavier than 10 pounds. Do not lift dumbbells or any heavy objects. Even something as simple as a grocery bag can put unnecessary strain on your abdominal muscles. Likewise, avoid exhausting your body with physical activities, as they may delay your healing.
3) Abdominal Exercises:
Any general surgeon in Navi Mumbai will strictly advise against abdominal exercises, such as situps, leg raises, crunches, and other activities that can strain your abdominal muscles. It’s best to hold off on these until your doctor gives you clearance.
Safe Alternatives
Instead of high-intensity workouts and weight training, you can consider these safer alternatives.
a) Gentle Walking:
Walking around your house is the best exercise for the first couple of days after surgery. It builds your muscle stamina. Start with a gentle walk using canes or walking aids, if recommended. Slowly, you can work your way up to a 20-minute walk without assistance.
b) Light Stretching:
Within a few weeks, you can incorporate light stretching into your routine. It improves your flexibility, reduces stiffness, and prepares your body for workout sessions. You can try a cat-cow stretch, seated forward bend, and standing side bends.
You can try other low-impact activities, like swimming and stationary cycling.
Tips for a Smooth Recovery
Recovery from hernia surgery can vary from patient to patient and usually depends on the type of surgery you’ve had and its complexity. Here are a few tips to ensure a smooth recovery after the procedure:
- Always consult your doctor before starting a new exercise
- Listen to your body and stop when you feel pain or fatigue
- Start slow
Conclusion
Establishing an exercise routine will speed up your healing and help you get back in shape. However, before proceeding, it’s important to talk to your surgeon about what’s safe and what to avoid.

How Many Rounds of Chemo is Normal?
Chemotherapy is one of the effective treatments for many types of cancer. These drugs, combined with radiation therapy, immunotherapy, hormone therapy, and surgery, are administered to prevent cancer from spreading and growing. A cancer specialist in Navi Mumbai recommends chemotherapy in multiple cycles.
This is to ensure that your body gets enough rest before the next cycle begins. It also helps assess how your body and the cancer responds to the medication. In this article, we’ve discussed all you should know about factors affecting chemotherapy duration, how many rounds of chemo is normal, and the chemo cycles. Let’s take a look:
Factors Influencing the Number of Chemo Rounds
The number of chemo sessions you need depends on many factors:
i) Type of Cancer:
Breast and lung cancer, for example, require 4-6 cycles of chemotherapy. Chronic leukemia may require ongoing chemo sessions that can last up to 2 years.
ii) Stage of Cancer:
Cancer that’s diagnosed at an early stage might require fewer chemo rounds compared to the advanced-stage cancer that’s spreading aggressively. Your treatment plan may include chemo sessions before and after surgery.
iii) Patient’s Health:
How your body reacts to the chemo drugs determine the number of chemo rounds required. If your tumor shrinks and your symptoms improve, the oncologist may recommend fewer sessions. If the progress is slow, more rounds might be scheduled.
Typical Chemotherapy Schedules
A normal range for chemotherapy rounds is between 4 and 6 cycles, but as mentioned above, it can vary from patient to patient, depending on the type and stage of cancer. Usually, the sessions start with chemo drugs, which are administered over a few days and are followed by a rest period of 2-3 weeks before another chemo session is planned.
Experts advise that chemotherapy drugs must be given with a rest period, as these medications can kill your fast-growing healthy cells. It’s a common side-effect of chemotherapy. So, while the treatment works wonders for cancer patients by killing the rapidly multiplying cancer cells, it also affects the cells responsible for your hair growth, cells in your mouth, gut, and other places. Your body needs adequate time to replenish these healthy cells.
Individualized Treatment Plan
Treatment is mostly personalized based on the patient’s age, type of cancer, and its aggressiveness. If needed, the chemotherapy regimen can be changed. The doctor decides whether to continue or how the future sessions should be planned based on how your cancer responds to the first few cycles.
Managing Side Effects
The most common side-effects after chemotherapy include fatigue, sore mouth, hair loss, nausea, vomiting, diarrhea or constipation, neuro pain, cognitive issues, weight loss, and low immunity.
Chemotherapy treatment in Navi Mumbai is associated with many side-effects, some of which can cause extreme discomfort and might interfere with your daily activities. Talk to your doctor if the side-effects get severe. They will recommend lifestyle modification, change medication, or switch your chemo regimen to manage side-effects. There’s no exact chemotherapy count. You may need only a couple of sessions to kill cancer completely. Others may need more for the best results.

Which Vaccines Are Given To Infants and Why?
Nobody likes to see their just-born baby getting vaccinated. However, immunization can prevent your babies from deadly diseases. A baby’s immune system is not fully developed, which puts them at an increased risk of certain illnesses and, eventually, hospitalization.
Many children die because of diseases that could have been easily prevented with vaccines. Your pediatrician in Navi Mumbai will give you a detailed list of the baby’s immunization schedule. We’ve compiled this detailed guide to help you understand different vaccines, the required dosage, and when they are given. Let’s see which vaccines are given to infants & why.
Vaccines Administered at Birth
1) Hepatitis B
It is the first shot administered to babies within 24 hours of life. The vaccine protects them from hepatitis B, a liver infection that’s highly likely to turn into a chronic liver illness if an infant contracts it. The vaccine is given right after birth to reduce the risk of the infant contracting the virus from the infected mother or other close ones. This vaccine is administered in three doses — one at birth, another in 1.5 months, and the last in 3.5 months.
2) Vaccines Given in the First Year
i) DTaP Vaccine:
Diphtheria, Tetanus, and Acellular Pertussis, short for DTaP, is a range of life-threatening illnesses that have killed many babies in the past. Diphtheria is a serious throat inflammation that can also lead to kidney and heart damage in young babies. Tetanus bacteria get into your body through an open wound. Pertussis is a whooping cough, particularly dangerous in babies.
ii) Hib Vaccine:
Haemophilus influenzae type b disease can cause serious brain or spinal infections in children under five. The Hib vaccine is administered in three doses (at 6 weeks, 10 weeks, and 14 weeks). It protects the baby from ear infections, throat inflammation, meningitis, and other serious infections.
iii) Polio Vaccine (IPV):
Polio vaccine protects babies from a deadly poliovirus that can result in paralysis and death. It’s also given in three doses.
iv) Pneumococcal Vaccine (PCV):
The pneumococcal vaccine protects babies from Streptococcus pneumoniae, a serious bacteria that can cause pneumonia, meningitis, and even sepsis in some cases.
v) Rotavirus Vaccine:
Rotavirus prevents diarrhea in infants. Severe diarrhea that causes frequent watery stools with fever, vomiting, and abdominal pain can cause dehydration in babies, and some need to be hospitalized. The vaccine is administered in 2-3 doses.
3) Vaccines Given Between 12 and 18 Months
a) MMR Vaccine:
The MMR vaccine is given in two doses, and once vaccinated, the child is protected from mumps, measles, and rubella for lifetime.
b) Varicella Vaccine:
Another vaccine included in the child’s routine immunization schedule is varicella for protection from chickenpox. The vaccine is administered in two doses and can mitigate the risk of disease severity or complications if the vaccinated child contracts it.
c) Hepatitis A Vaccine:
Hepatitis A vaccine offers life-long protection from the viral infection that can cause liver diseases. It spreads through an infected person or by ingesting contaminated food.
Conclusion
Children’s immunization in Navi Mumbai is done at private pediatric and government hospitals. It’s important to keep track of your child’s vaccination schedule and get every dose at the right time.
What Happens to the Uterus After Uterine Artery Embolization?
Women experiencing heavy bleeding due to uterine fibroids, malignant growth, and other medical conditions can opt for Uterine Artery Embolization treatment in Navi Mumbai. It’s a less-invasive alternative to open uterus surgery for removing fibroids and the uterus. The procedure cuts the blood supply to the fibroids, making them shrink and eventually die. This is also an effective way to control excessive bleeding. The question is, what happens to the uterus after uterine artery embolization? Let’s find out.
Immediate Aftereffects
You will be given sedatives and medication that numbs your groin area. So, you won’t feel a thing during the procedure. You are supposed to lie straight for 5-6 hours. Afterward, when the effect of the anesthesia wears off, you might experience mild cramping and some discomfort. Your doctor will prescribe pain medication. The pelvic pain can be moderate or severe for the first few days following the UAE.
Short-term Changes
The major goal of the procedure is to reduce the fibroid size and control heavy bleeding. Here’s what you can expect during recovery:
a) Reduction in the Fibroid Size:
After the procedure, the blood supply to the fibroid is cut off, and their size will gradually decrease. It may take weeks or months for them to die, though. If the fibroids are located close to the uterine lining, they might expel through your vagina. You can expect some bleeding if that happens.
b) Pelvic Pain Relief:
Once the fibroids die, you will notice an improvement in your pelvic pain. Women with urinary incontinence due to fibroids putting pressure on the bladder will also notice improvement in their symptoms.
c) Regulate Menstrual Cycles:
After UAE, you may notice slight bleeding and skip periods for a few weeks. Your periods will gradually return, initially with light bleeding and then regular menstrual bleeding. This will be better and comparatively lighter than the pre-procedure state.
Long-term Outcomes
Although the procedure’s outcome is great, with patients reporting no heavy bleeding after UAE, it does come with its share of risks.
A) Fertility Issues:
It’s possible to get pregnant after UAE, but it comes with an increased risk of miscarriage and preterm birth. It’s best to talk about the potential complications with your gynecologist.
B) Additional Treatment:
UAE is very effective, but there’s a chance the fibroids will return or the existing ones will not die completely. If the treatment doesn’t work, you may need to consider surgery for fibroid removal or hysterectomy.
When to See Your Doctor?
Pelvic pain is not uncommon after the UAE. It can start in 24 hours and may last a few days. You can take over-the-counter painkillers to relieve pelvic discomfort. However, if the pain persists or is too severe to let you perform routine tasks or work, report it to your doctor. Other unusual symptoms after UAE are a high-grade fever with a vaginal discharge (this might indicate an infection) and heavy bleeding.
Conclusion
The process is safe overall, but it’s better to stay in touch with your gynecologist and watch for the warning signs mentioned above. Once you’ve had uterine artery embolization, it’s only a matter of time before you can resume your work like usual.
Sleeping Position After D&C
Dilatation and curettage (D&C) treatment in Navi Mumbai is a minimally invasive surgical procedure in which the doctor uses medicine or tools to open your cervix and insert instruments that scrape the uterine surface. This removes the uterine tissues. A suction can also be used for the procedure.
Although there’s no specific sleep position for a D&C patient, some positions can help you get good quality sleep. Below, we’ve discussed the best sleeping position after D&C.
Recommended Sleeping Positions
a) Sleeping On Your Back
This is the most comfortable position for a woman who has just gone through D&C. It doesn’t put pressure on your abdomen, allowing your body, especially the pelvic region, to heal after surgery. It also provides relief from cramping and discomfort. Sleeping on your back is also good for blood circulation. The better your blood circulation, the faster you will heal.
b) Sleeping On Your Side
Another doctor-recommended sleep position after D&C is on your side. Side sleeping (left and right) is considered safe and a good option for women experiencing mild cramping, bloating, and back pain. It also promotes good blood flow, which supplies nutrients to the healing tissues, speeding up your recovery.
Positions to Avoid
A) Sleeping On Your Stomach
Gynecologists in Navi Mumbai do not recommend this position, as it puts unnecessary strain on your abdomen and pelvis. As your uterus contracts and goes back to its normal size, it may cause cramps. To relieve the pain, it’s advisable to sleep in a position that feels relaxing.
B) Sleeping in a Curled-up Position
While it may feel comfortable to get curled up like a fetus in a mother’s womb, it’s not a safe position after D&C. It brings your knees close to your chest, which may strain your abdominal and pelvic muscles. It can make your cramping worse and increase discomfort. Besides, this sleep position has many side effects, like joint stiffness, muscle ache, difficulty breathing, back strain, and so on.
Tips for Comfort
1) Using Supportive Pillows
Consider adding a pillow under your knee and the back to prevent back strain and abdominal pain after surgery. You can also hug a pillow to get chest support. Pillows under your legs will keep your spine in the most comfortable position while you sleep.
2) Maintaining the Right Environment
In addition to the sleep position, the sleep environment matters. Turn off your phone, remove distractions, turn off the lights, and keep the room’s temperature comfortable. Creating a cozy environment will help you fall and stay asleep.
3) Listen to Your Body
If you feel pain or your symptoms get worse in any sleeping position, switch immediately.
Conclusion
D&C is mainly performed on women who want an abortion or suffer a miscarriage. The procedure can also be used for testing. It can detect uterine fibroids, polyps, and other uterine-related issues that cause abnormal bleeding, pelvic pain, and other unusual symptoms. It’s a relatively safe procedure, but a good sleep position with a balanced diet and a proper exercise routine is crucial for quick recovery.