What Is the Best Treatment for Piles?
Introduction to Piles
Nearly three out of four adults suffer from piles. It can cause discomfort, pain, itching, and bleeding. Hence, it is essential to seek appropriate treatment. Generally, piles, or hemorrhoids, are swollen blood vessels in the rectal and anal areas. They can be internal, occurring inside the rectum, or external, forming under the skin around the anus. Here, you can explore the causes, symptoms, and Piles Treatment Hospital in Navi Mumbai. You can also learn about thediagnosing methods, treatment options, and prevention tips for piles.
Causes of Piles
Several factors contribute to the development of piles, including:
- Chronic constipation and straining during bowel movements are common causes.
- Prolonged sitting or standing, obesity, pregnancy, and a sedentary lifestyle can also increase the risk.
- Additionally, a family history of piles and aging are known risk factors.
Symptoms of Piles
The symptoms of piles can vary depending on their type and severity. Internal piles may cause painless bleeding during bowel movements, while external piles can lead to pain, swelling, itching, and discomfort. In some cases, blood clots may form in external piles, causing a painful condition called thrombosed hemorrhoids. However, you must see a Piles Doctor in Navi Mumbai if you find any symptoms.
Diagnosing Piles
At Mangal Prabhu Hospital, a medical professional physically examines the anal area to diagnose piles. It usually involves a visual inspection, but sometimes needs a digital rectal examination to assess the rectum. In some cases, doctors recommend additional diagnostic procedures like sigmoidoscopy or colonoscopy to rule out other potential causes.
Also Read: Understanding The Different Types Of Surgeries: A Guide For Patients
Treatment Options for Piles
The piles’ treatment aims to alleviate symptoms, reduce swelling, and promote healing. You can receive the following treatment approach for piles at Mangal Prabhu Hospital:
i) Lifestyle Modifications
Making changes to your lifestyle can help manage and prevent piles. These include maintaining a high-fiber diet, drinking plenty of water, exercising regularly, and avoiding prolonged sitting or standing.
ii) Topical Medications
Over-the-counter creams, ointments, or suppositories containing ingredients such as hydrocortisone, witch hazel, or lidocaine can temporarily relieve pain, itching, and inflammation.
iii) Oral Medications
Doctors may recommend pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), to reduce pain and inflammation.
Prevention Tips for Piles:
Here are some preventive measures for the occurrence or recurrence of piles, including:
1. Maintain a High-Fiber Diet
A diet rich in fiber helps soften the stool, making it easier to pass without straining. Include fruits, vegetables, whole grains, and legumes daily.
2. Stay Hydrated
Drink adequate water throughout the day to keep stools soft and prevent constipation.
3. Regular Exercise
Engage in regular physical activity to promote healthy bowel movements and improve circulation.
4. Avoid Straining
Do not strain during bowel movements. Use a stool softener or try a different position, such as squatting, to make the process easier.
Conclusion
The treatment of piles depends on the severity of the condition and the individual’s specific circumstances. Lifestyle modifications, like dietary changes, are crucial in preventing and managing piles. You must consult a healthcare professional for an accurate diagnosis and personalized treatment plan for piles. Individuals can effectively manage piles and improve their quality of life by following the appropriate treatment options and preventive measures.

Fibroid Removal Surgery: Understanding the Potential Side Effects
What is Fibroid Removal Surgery?
Many people with uterine fibroids undergo fibroid removal surgery. They are noncancerous growths that develop in or around the uterus. Fibroid Removal Surgery in Navi Mumbai alleviates symptoms such as heavy menstrual bleeding, pelvic pain, and fertility issues. It is also known as myomectomy. Here you can explore the causes of fibroids, different types of fibroid removal surgery, and other vital insights.
Causes of Fibroids
The exact cause of fibroids is unknown. But, several factors contribute to their development, including:
- Hormonal imbalances
- Genetic predisposition
- Estrogen dominance
- Hormonal fluctuations, such as those occurring during pregnancy or with hormone replacement therapy, can promote fibroid growth.
Types of Fibroid Removal Surgery
At Mangal Prabhu Hospital, you can get several fibroid removal surgery options, including:
1. Abdominal Myomectomy
This procedure involves making a larger incision in the abdomen to access and remove fibroids.
2. Laparoscopic Myomectomy
Laparoscopic myomectomy is a minimally invasive procedure in which a Fibroid Surgeon in Navi Mumbai makes small incisions in the abdomen to insert a laparoscope and other surgical instruments.
3. Hysteroscopic Myomectomy
Surgeons perform this myomectomy through the vagina and cervix without any external incisions. A hysteroscope, a thin tube with a light and camera, is used to visualize and remove fibroids.
Also Read: Understanding The Role Of An OB-GYN In Women’s Health
Potential Side Effects:
While fibroid removal surgery can relieve symptoms, you must understand and be prepared for potential side effects. These can include:
i) Pain and Discomfort
It is common to experience pain and discomfort after the surgery.
ii) Bleeding and Infection
Some women may experience vaginal bleeding or discharge following the surgery. In rare cases, infection may occur, characterized by fever, increased pain, or abnormal discharge.
iii) Scarring
All surgical procedures involve the risk of scarring.
iv) Adhesion Formation
Adhesions are bands of scar tissue that can form between organs or tissues. Sometimes, fibroid removal surgery may lead to the formation of adhesions. It can cause pain or affect fertility.
Tips for Recovery
Mangal Prabhu Hospital suggests following these tips to facilitate a smooth recovery from fibroid removal surgery, including:
a) Follow Post-Surgery Instructions
Adhere to all post-surgery instructions provided by your healthcare provider, including medications, wound care, and activity restrictions.
b) Rest and Allow Your Body to Heal
Take ample rest and avoid strenuous activities during the initial recovery period. Gradually increase physical activity as advised by your healthcare provider.
c) Maintain a Healthy Diet
Eat a nutritious diet rich in fruits and proteins to support healing and overall well-being.
d) Stay Hydrated
Drink plenty of water to stay hydrated and promote optimal healing.
e) Attend Follow-Up Appointments
Regularly attend follow-up appointments with your healthcare provider to monitor your recovery and address any concerns or complications.
Conclusion:
Fibroid removal surgery can provide relief from the symptoms associated with uterine fibroids. While the procedure is generally safe and effective, knowing the potential side effects and preparing for proper recovery is essential. By understanding the causes of fibroids and the different types of fibroid removal surgery, you can make informed decisions. It will improve the chances of a successful surgical outcome. You must also consult with a healthcare provider to discuss specific risks, benefits, and expected outcomes based on your circumstances.

What Are Some Treatments For Hypertension?
What is Hypertension?
Nearly half of adults worldwide have hypertension. Individuals with this condition have significant risk factors for various cardiovascular diseases. It can lead to serious health complications if you leave it unmanaged. Hence, you can also explore its causes, methods of diagnosis, and various available Hypertension Treatment in Navi Mumbai. This blog helps you learn more about hypertension.
Causes of Hypertension
Some factors can lead to the development of hypertension. Here are a few factors, including:
- Genetics
- Certain conditions like diabetes and sleep apnea
- Unhealthy lifestyle habits
Diagnosis of Hypertension
A General Physician in Navi Mumbai diagnoses hypertension by measuring blood pressure. They use a blood pressure cuff and a stethoscope or an automated blood pressure monitor. Consistently elevated blood pressure readings above the normal range may indicate hypertension.
Treatments for Hypertension
Mangal Prabhu Hospital aims to lower blood pressure levels and reduce the risk of associated complications using the following treatment for hypertension:
Lifestyle Changes
Lifestyle modifications play a crucial role in managing hypertension. These include:
- Emphasize fruits, whole grains, and low-fat dairy products. And limit sodium, saturated fats, and added sugars.
- Engage in moderate aerobic exercise for at least 150 minutes or vigorous exercise for 75 minutes per week.
- Achieve and maintain healthy body weight through healthy eating and physical activity.
- Practice stress management techniques such as deep breathing exercises, or meditation to reduce stress levels.
Also Read: Why It Is Important To Have Preventive Health Check-ups?
Medication
Sometimes, lifestyle changes alone may not be sufficient to manage hypertension. Doctors at Mangal Prabhu Hospital may prescribe medications to lower blood pressure levels. Commonly prescribed medications include:
- Diuretics
It promotes urine production, reducing fluid volume and lowering blood pressure.
- ACE Inhibitors and ARBs
It helps relax blood vessels and inhibit the effects of hormones that narrow blood vessels.
- Calcium Channel Blockers
It prevents calcium from entering the muscle cells of the heart and blood vessels, relaxing them and reducing blood pressure.
- Beta Blockers
It reduces the workload on the heart and blocks certain stress hormones to lower blood pressure.
Alternative Treatments
Complementary and alternative therapies may be used as adjunctive approaches to manage hypertension. These include:
- Acupuncture
It involves the insertion of thin needles into specific points on the body. It promotes relaxation and improves blood flow.
- Biofeedback
It helps individuals gain control over their body’s physiological responses, such as heart rate and blood pressure. It involves relaxation techniques and mental exercises.
- Mindfulness-Based Stress Reduction
It combines meditation, yoga, and other mindfulness practices to reduce stress.
Conclusion: Strategies for Managing Hypertension
Managing hypertension requires a comprehensive approach that includes lifestyle modifications, medication when necessary, and alternative treatments. Adapting a healthy lifestyle can significantly contribute to blood pressure control. Medications may be prescribed to lower blood pressure levels when lifestyle changes alone are insufficient. Moreover, alternative therapies like acupuncture can be beneficial as adjunctive treatments.
Individuals with hypertension must work closely with healthcare professionals. They will help them develop a personalized treatment plan considering their needs and medical history. By implementing these strategies, You can effectively manage hypertension and reduce the risk of associated complications.
Understanding Neonatal Intensive Care: What Parents Need to Know
What is Neonatal Intensive Care, and why is it essential?
Neonatal intensive care, or NICU, is a rare medical unit that provides 24/7 care for newborns with extreme medical conditions. It is a nursery in a hospital that provides round-the-clock care for ill or preterm babies. It has healthcare facilities that give special training to give your baby the best care. You can visit Neonatologists in Navi Mumbai as they provide these facilities.
What to Expect When Your Baby is in the NICU?
NICU Hospital in Navi Mumbai provides intensive care for newborns facing medical challenges. Having a baby in Neonatal Intensive Care can be a formidable experience for parents. Knowing what to expect during this time can help relieve anxiety and encourage parents to participate in their baby’s care actively. Things to expect when your baby is in NICU:
- A team of skilled healthcare professionals will actively and closely monitor your baby’s progress. The Neonatologist, NICU staff, and professionals will provide round-the-clock care and check if your baby’s needs are met.
- You can expect an explanation of medical procedures and equipment that is being used.
- Their environment will focus on infection control and safety, like using hygiene protocols to protect the infants.
- Your baby’s stay in the NICU depends on their medical condition and response to treatment. It’s better to celebrate the event and stay comforted knowing that NICU is providing care for your baby.
- The NICU treatment can be emotionally challenging for almost every parent. Reach out to the NICU staff for support groups where you can connect with families that are facing the same experience.
Also Read: NICU And PICU: What Is The Difference?
How to Support Your Baby During Their Stay?
Parents find it challenging to have a baby in the neonatal intensive care unit/NICU. Parents also play an essential role in their baby’s development during this time. The List below explains some of the ways to support your baby during their stay:
- To connect through touch, like skin-to-skin contact, also known as kangaroo care. Kangaroo care has shown benefits for premature infants. Gently pulling your baby against your chest promotes bonding.
- Be an advocate for your baby; creating soft sounds can provide comfort.
- Bring familiar items like small toys or swaddles. Maintain routine and establish connections even in hard times.
Tips for Dealing with the Stress of Having a Baby in the NICU
- Educate yourself about the baby’s condition
- Try to celebrate milestones
- Write your thoughts as a therapeutic outlet
- Have patience, and remember that the journey may have ups and downs, and healing takes time.
Long-Term Outlook for Babies in the NICU
Babies that received exceptional care in the NICU from Mangal Prabhu Hospital have a confirmed long-term outlook. Advanced and comprehensive interventions have improved chances of healthy growth and thriving in their future attempt.
Conclusion
Understanding NICU is essential for parents facing the challenging journey of having a baby in critical condition. Mangal Prabhu Hospital provides specialized medical care and a dedicated healthcare team to support newborns. Parents play an essential role in their baby’s recovery by being involved in their care.

Lifetime Precautions After a Hip Replacement
Generally, seniors undergo hip replacement surgery to improve mobility and reduce pain. If you know someone undergoing this surgery, you must ensure they know the lifetime precautions. The Hip Replacement Surgeon in Navi Mumbai educates its patient about lifetime precautions after their procedure. Individuals can ensure a successful and long-lasting outcome by following these precautions and taking care of the new joint. In this blog, you can explore the essential lifetime precautions after a hip replacement.
Understanding the Lifetime of a Hip Implant
Before learning about the lifetime precaution, let’s learn about the lifetime of the hip implant. These implants can vary in material and design. The lifespan of hip implants depends on multiple factors, such as their type and the individual’s lifestyle. On average, most hip replacements continue to function well even after ten years, and many can last a lifetime. You must consult with the surgeon from Orthopedic Hospital in Navi Mumbai about the specific characteristics of the implant and its expected longevity to ensure appropriate care.
Precautions to follow after Hip Replacement Surgery
People with hip replacement surgery should follow these precautions from Mangal Prabhu Hospital, including:
1. Crossing Legs and Twisting Movements
Avoid crossing legs and twisting movements, including pivoting on one leg and walking pigeon-toed, should be avoided to minimize the risk of dislocation. Side sleepers may find sleeping with a pillow between their legs beneficial to maintain proper alignment. It’s important to be mindful of these movements and make conscious efforts to protect the hip joint.
2. Bending Too Far
Excessive hip flexion can lead to dislocation, so seniors should avoid bending the hip joint beyond 90 degrees. Activities like putting on socks or shoes should be done with caution. Choosing appropriate seating, like chairs with the thighs parallel to the floor, helps maintain the correct angle. Tall individuals may need elevated cushions for chairs or toilet seats to prevent over-bending.
Also Read: How To Sleep After ACL Surgery?
3. Repetitive, High-Impact Activities
While exercise is essential for maintaining muscle tone and balance, certain activities can strain the hip implant excessively. Repetitive motions and high-impact exercises like running and jumping should be avoided. Instead, low-impact exercises such as swimming, yoga, and stationary biking are recommended to restore range of motion without risking damage to the implant.
4. Air Travel Considerations
If the hip implant contains metal, it may set off metal detectors at airport security checkpoints. Informing the TSA agent about the presence of a metal hip implant is advisable. Full-body scanners are usually more effective at detecting internal metal. Still, even if the alarm sounds, it’s typically resolved with a physical pat-down or electromagnetic wand screening to ensure safety.
Conclusion
By following the lifetime precautions after a hip replacement, individuals can maintain the integrity of their new joint and enjoy a fulfilling life. Seniors should prioritize low-impact exercises and be aware of air travel considerations. Elderly people also avoid excessive bending and twisting. It will contribute to the long-term success of hip replacement surgery. Consult healthcare professionals at Mangal Prabhu Hospital for personalized advice throughout the journey. They will help you manage your pain and prevent complications.
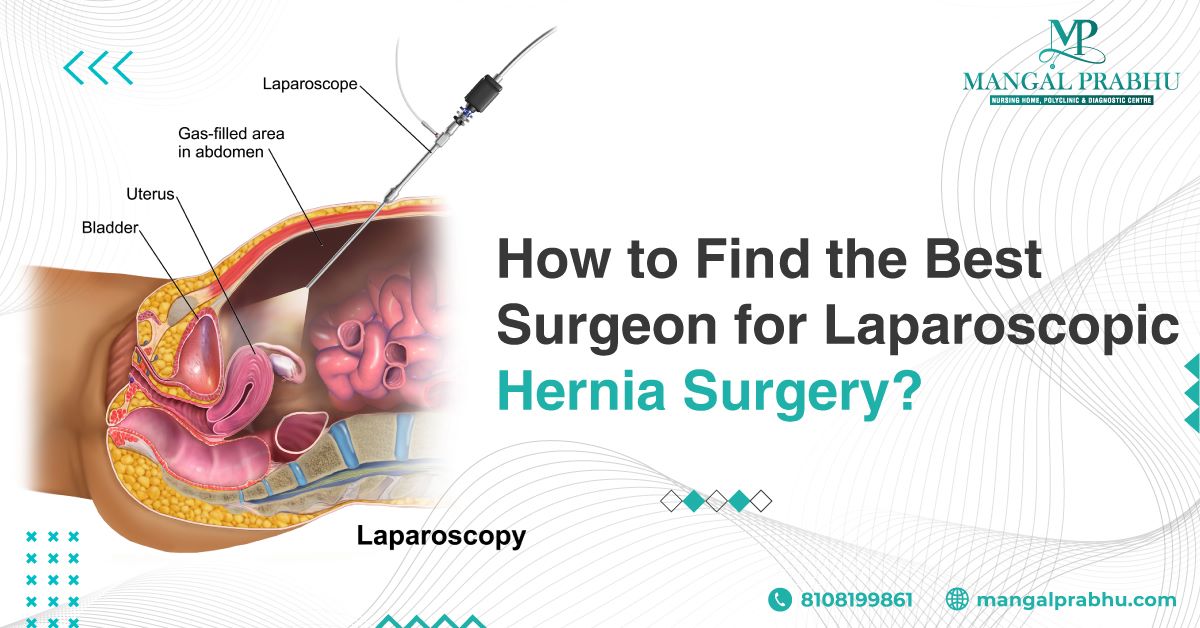
How to Find the Best Surgeon for Laparoscopic Hernia Surgery?
Finding the best surgeon for laparoscopic hernia surgery is a difficult step for having a successful and safe procedure. This blog offers valuable tips for finding the best hernia surgery surgeons in Navi Mumbai. Follow the right method and increase your successful treatment rate.
What is Laparoscopic Hernia Surgery?
Hernia surgery includes using a laparoscope, a thin fiber-optic instrument/tube equipped with a camera. The surgeon cuts the abandonment around the hernia site, and the laparoscopy is inserted through the cut to provide a clear view of the area. The hernia is then repaired using webbing and stitches by which the cuts are closed. You can visit Mangal Prabhu Hospital for this surgery as they have excellent professionals.
Benefits of Laparoscopic Hernia Surgery
Hernia surgery has become so popular Hernia Treatment in Navi Mumbai these days because of its benefits. Some of the benefits of hernia surgery include:
1. Reduction in Pain:
Small cuts in laparoscopic surgery result in less damage compared to general traditional open surgery
2. Faster Recovery:
Since there are small incisions in surgery, the recovery from surgery is way quicker than open surgery
3. Minor Scars:
Laparoscopic surgery doesn’t leave prominent scars, compared to open surgery, which has minimal scars
4. Chances of Fewer Infections:
Laparoscopic surgery reduces the chances of risk of wound infections and other complicated infections
5. Fewer Chances of Recurrence of Hernia:
Laparoscopic techniques have been associated with less rate of recurrence of hernia.
How to Choose a Surgeon for Laparoscopic Hernia Surgery
You must carefully consider a few factors to choose the best surgeon for laparoscopic hernia surgery. Here are some things to consider while looking for a surgeon for laparoscopic surgery.
i. Surgeon’s Qualifications:
Verify the surgeon’s qualifications and certification and check whether he has done training and has experience in laparoscopic hernia surgery.
ii. Experience:
You can inquire about the Surgeon’s Experience. A surgeon with multiple surgeries is likely to have better skills and experience. At Mangal Prabhu Hospital, you can find experienced surgeons who offer excellent treatment for hernias.
iii. Hospital Affiliations:
Hospital affiliations play an essential role. Look for hospitals with better facilities, advanced technologies, and high standards.
Also Read: How To Prevent Hernia?
Questions to Ask Your Laparoscopic Hernia Surgeon
While looking for a surgeon, you must ask him several questions, such as:
- How many laparoscopic hernia surgeries they had performed?
- What is their success rate in terms of hernia repair and recurrence?
- How do they determine if a patient is suitable for laparoscopic hernia surgery?
- What is their preferred technique for laparoscopic hernia repair, and why?
- What measures do they take to ensure patient comfort during and after the procedure?
Tips for Choosing the Right Surgeon
- Ask others’ opinions, as it is better to take others’ opinions while searching for a surgeon.
- Trust the surgeon as trusting them is necessary to find a good surgeon.
- You must ensure your surgeon is willing to listen to what you say to him.
- The location of surgeons’ practice and easy access to the hospital.
Conclusion
Choosing the best Laparoscopic Hernia Surgeon in Navi Mumbai is a hard decision that can affect your overall experience and the outcome of the surgery. You must take the time to research and choose the best hospital and best surgeon.

Understanding Vaginal Birth After Cesarean (VBAC)
Women who have had a cesarean section, often wonder if they can have a vaginal birth next time. The good news is that you can opt for vaginal birth. Studies show that VBAC has a success rate. Here, you can learn the vaginal birth after cesarean. You can talk with a gynecologist in Navi Mumbai to decide if VBAC is right for you.
Definition of Vaginal Birth After Cesarean (VBAC)
Vaginal Birth After Cesarean is commonly known as VBAC. This procedure refers to the delivery of a baby through the vagina by a woman who has previously undergone a cesarean section for a previous birth. It allows women with a prior C-section to experience a vaginal birth for subsequent pregnancies. You can visit Mangal Prabhu Hospital if you want this medical procedure. They are known for their skilled medical professionals and complete care.
Benefits and Risks of VBAC
VBAC presents several potential benefits for women. It allows them to avoid the risks associated with repeat C-sections, such as infection, blood loss, and more. Vaginal birth also facilitates a quicker recovery and a lower risk of future surgical complications. Additionally, it promotes a sense of empowerment and satisfaction for women who desire a more natural birth experience.
However, this procedure also carries certain risks. The most significant concern is uterine rupture, which occurs when the scar from the previous C-section opens during labor. Although the risk is relatively low, it can be life-threatening for both the mother and the baby.
Factors That Affect VBAC Success
Several factors influence the success of a VBAC. The primary consideration is the type of uterine incision from the previous C-section. Low transverse incisions are associated with higher success rates for VBAC, while vertical incisions pose a greater risk of uterine rupture.
Other factors include:
- The reason for the previous C-section.
- The interval between pregnancies.
- The mother’s age.
- The estimated weight of the baby.
- Certain medical conditions.
The support of a healthcare provider experienced in VBAC, and a suitable birthing environment also contributes to a higher likelihood of success.
Also Read: The Role of an OB-GYN in Women’s Health
Preparing for VBAC
Visit a Maternity/Pregnancy Hospital in Navi Mumbai that provides excellent healthcare services for expectant mothers. They can help you get prepared for VBAC. However, you can follow these tips to increase the chances of a successful VBAC:
- Review details of the previous C-section
- Assess current pregnancy
- Discuss potential risks or concerns
- Regular prenatal check-ups
- Monitor baby’s growth and position
- Address medical conditions
The Delivery: What To Expect
When the delivery time approaches, the VBAC process is similar to that of spontaneous vaginal birth. Women may experience labor pains, and contractions, and progress through the stages of labor. However, continuous monitoring of the mother and baby is necessary to ensure their safety.
Conclusion
If you are seeking a gynecologist in Navi Mumbai, Mangal Prabhu Hospital is a reputable choice. They can perform VBAC. It offers women the opportunity to have a vaginal birth after a previous C-section, offering potential benefits. Women can make informed decisions about their birthing options by understanding the benefits, risks, and necessary preparations.
How to Reduce Appendix Pain?
The appendix is a small pouch attached to your intestine at the lower right side of your abdomen. The appendix can get blocked, causing the bacteria inside it to multiply rapidly, filling it with pus. As a result, it can get inflamed, requiring surgery.
Appendicitis can be life-threatening if the appendix bursts, spreading the bacteria to the abdominal cavity. You must get immediate appendix removal treatment in Navi Mumbai to prevent complications. Read on to learn more about appendicitis, when you need an appendectomy treatment, and how to relieve the appendix pain.
Examining the Symptoms of Appendix Pain
Appendicitis pain is extremely severe. It starts with mild cramps in your upper and lower abdomen, especially around the belly button. The pain is often described as a sharp and sudden pinch in the abdomen.
It gets worse when you move. The pain is so severe that you won’t be able to fall or stay asleep at night. The worst part is appendicitis requires almost immediate medical attention, i.e. within 24-48 hours. The pain keeps getting worse every hour. Here are some other symptoms of appendicitis.
- Loss of appetite
- Nausea and vomiting
- Fever
- Indigestion
- Diarrhea
If you feel constipated, do not use an enema, laxatives, or any medication or tool to pass the bowel movement. This can burst your appendix.
Also Read: Understanding The Different Types Of Surgeries: A Guide For Patients
Ways to Help Reduce Appendix Pain
Unfortunately, you cannot get rid of the appendicitis pain, as it tends to get worse over time. Painkillers might help for a while, but that’s only until their effect lasts. It’s best to see a general surgeon in Navi Mumbai and get an appendectomy—a surgery to remove your appendix.
Since the appendix is not an essential organ and one can easily live without it, having it surgically removed is the only treatment option for appendicitis. It’s usually performed as an emergency treatment.
Here’s what you should do to avoid complications after the surgery:
1. Limit Strenuous Activities:
Do not practice any strenuous activity that puts unnecessary pressure on your abdomen or the site of the operation. If the surgery was performed laparoscopically, you can start moving 3-4 days after the operation, however, open surgery involves a longer recovery period.
2. Use Support When Moving:
Place a soft pillow on your abdomen and hold it gently when you cough, laugh, or move.
3. Contact Your Doctor:
If you still feel sharp or mild pain, contact your doctor immediately to seek medical help.
4. Rest:
Take leave from work or your classes for one week. You need rest post-surgery to speed up the healing. Take short walks initially. You can return to work when you feel alright. It’s best to talk to your doctor about when you can resume your work. Avoid strenuous activities for at least a month, so that your body can heal faster.
Conclusion
Appendicitis is an emergency medical condition that requires immediate treatment. If you notice the above-mentioned symptoms, contact a doctor immediately. Usually, people don’t have much time to prepare for appendectomy, as the surgery is an emergency treatment that’s performed during diagnosis.

How to Recognize, Treat, and Prevent Urinary Tract Infections (UTIs)?
A urinary tract infection is often caused by the Bacteria E. coli. It is one of the most common types of infection that can occur in any part of your urinary tract system. The condition can involve your kidneys, bladder, urethra, and other organs in your urinary tract. It’s important to see a urologist in Navi Mumbai if you’ve developed UTI.
Your urinary system makes and stores pee, which consists of the waste products and the excess fluid in your blood. It usually passes through your urinary tract without causing contamination or leaving any bacteria, but sometimes, the bacteria can enter your urinary system causing UTI. Read on to learn more about UTI, its causes, symptoms, and treatment.
Causes and Symptoms of UTIs:
UTI is caused by the bacteria that enter your urinary tract system through the urethra and spread across the bladder and other organs. Your immune system is designed to keep these bacteria out of the urinary system, but they can fail sometimes, causing these microorganisms to multiply.
The infection can cause inflammation in your urinary tract, which may cause the following symptoms:
- Pain in the lower back
- An unusual odor from the pee
- Frequent trips to the bathroom
- Pain while peeing
- Blood in the pee
Some people may experience nausea, vomiting, fever, fatigue, and pressure in the pelvic area.
How to Recognize a UTI?
If you experience the above symptoms, head to the urology hospital in Navi Mumbai and share your symptoms with the healthcare provider. The doctor will take the urine test where they collect the sample of your urine and send it for testing in the lab. Or, they will order an ultrasound to get a closer look at your internal organs. Cystoscopy and CT scans are other common tests that can help detect a urinary tract infection.
Also Read: When Should I See A Urologist?
How to Treat a UTI?
A combination of antibiotics is prescribed to treat UTIs. It’s important to follow your doctor’s instructions carefully and take antibiotics as recommended. Missing a dose or stopping it once your condition improves can cause the infection to return. Usually, doctors give low-dose antibiotics, as people can develop resistance to this medication, making it difficult to treat the UTI.
If the antibiotics do not work or the infection has spread to the kidneys, you might require immediate intravenous treatment, where the doctor gives the medication through a needle inserted into your veins. You need to continue antibiotics after returning from the hospital.
How to Prevent UTIs?
Yes, it’s possible to reduce the risk of developing UTIs. Here are the tips that may help:
- Practice good hygiene
- Drink enough water
- Pee right after having sex, as bacteria can move into your urethra after intercourse.
- Avoid tight-fitting clothing
- Use water-based lubricant during intercourse
- Pee frequently
Conclusion
UTIs are treatable and preventable. The infection can be treated with the right antibiotics. The symptoms can get irritating, but with some changes in lifestyle and regular medication, you can get rid of the infection.
Tips to Reduce Pulmonary Fibrosis Risk!
Pulmonary fibrosis is a lung disease that thickens your lung tissues and causes scarring. The disease affects the lung, the surrounding tissues, and the air sacs, affecting the ability of the lungs to expand normally. As a result, the patient experiences difficulty breathing, dry cough, and fatigue.
You can see a general physician in Navi Mumbai to identify the symptoms of pulmonary fibrosis and figure out the most suitable treatment. However, the condition has currently no cure. We’ve listed some ways you can reduce the risk of developing the disease. Let’s take a look.
How To Reduce the Risk of Pulmonary Fibrosis
Unfortunately, there is no certain way or a proven method to prevent pulmonary fibrosis, but a few right steps can reduce your risk of developing the condition and managing it if you are already diagnosed with this lung disease. Here’s what may help.
1. Avoid Dust Exposure
One of the many risk factors for developing pulmonary fibrosis is exposure to dust and fumes. Working in a place where you are exposed to dust can put you at an increased risk of respiratory diseases, which can eventually result in pulmonary fibrosis. To lower your risk of the condition, it’s advisable to avoid exposure to dust and other harmful elements as much as possible.
2. Quit Smoking
Smoking causes inflammation in your lungs and creates thick mucus, which increases your risk of developing chronic lung diseases, lung cancer, and pulmonary fibrosis. Not just that, but smoking can make the disease worse. If you have pulmonary fibrosis, you must quit smoking right away to prevent the disease from worsening.
3. Get Treatment for Lung Infections
Chronic lung diseases develop gradually and worsen over time when left untreated. It’s important that you see a doctor if you notice any signs of infection. Infections like flu and pneumonia can weaken your lungs, making them vulnerable to chronic lung conditions. Getting vaccinated for such conditions is important to reduce the risk of pulmonary fibrosis and other lung diseases.
Also Read: COPD: Symptoms And Stages
Treatment for Pulmonary Fibrosis
While there is no permanent cure for pulmonary fibrosis, you must visit the pulmonology treatment center in Navi Mumbai to discuss the treatment options for managing the disease and slowing its progression.
- Oxygen Therapy: If the levels of oxygen are found in lower than normal volume, the healthcare expert might recommend you get oxygen therapy either through the oxygen tank or nasal cannula. However, it doesn’t cure pulmonary fibrosis. The therapy can improve your quality of life by managing your symptoms and helping you breathe comfortably.
- Medication: Based on your health, you might be advised to take certain medications to get relief from the symptoms of pulmonary fibrosis. Immunosuppressants and bronchodilators are commonly prescribed to patients at risk of developing lung conditions or those diagnosed with chronic lung disease.
- Lung Transplant: In some cases, a lung transplant might be needed to recover from the condition. If your lungs have been severely damaged, the doctor will advise you to replace them with healthy donor lungs.
Conclusion
The prevention of pulmonary fibrosis is essential for preserving respiratory health and overall well-being, to sum up. People can significantly reduce their risk of developing pulmonary fibrosis by adhering to the advice provided in this blog, such as quitting smoking, avoiding dust exposure, and seeking early medical intervention for any respiratory symptoms.
Always remember that prevention is always preferable to treatment and that protecting your lungs is an investment in your long-term health. Remain informed, look after your respiratory system, and put your health first. By doing this, you can live a healthier life and lower your risk of developing pulmonary fibrosis.