What are the Kidney Disease Symptoms in Females?
Kidney disease or kidney failure occurs when your kidney stops functioning. It’s usually the gradual loss of normal function, which results in its inability to filter waste from your blood. Kidney disease can be a life-threatening condition, as it can result in the excess buildup of electrolytes and waste in your blood.
If you experience a problem with urination, see a kidney specialist/nephrologist in Navi Mumbai to rule out the possibility of kidney failure. Your healthcare provider might recommend medication to slow down the damage, but eventually, you will need dialysis or a kidney transplant.
Symptoms of Kidney Disease
Kidney disease develops slowly in men and women. The symptoms usually don’t appear until it has reached an advanced stage. Based on the severity of the condition, here are some common symptoms that women diagnosed with kidney disease might experience.
- Nausea and vomiting
- Swollen ankles and feet
- Dry skin
- Hypertension
- Shortness of breath and chest pain if the excess fluid accumulates in your chest
- Frequent urination
- Insomnia
- Feeling dizzy
- Inability to concentrate or think clearly
- Brownish or reddish urine
- Bubbly urine
As mentioned previously, it’s advisable to see a doctor immediately if you notice any change in the pattern of urination, blood pressure, and swelling in the ankle. Kidney diseases do not produce severe symptoms unless the damage has reached the irreversible stage.
Also Read: How Stones Are Formed In Kidney?
Diagnosis of Kidney Disease
Chronic kidney disease can be diagnosed with a routine blood and urine test. The test is recommended for people with diabetes, hypertension, kidney injury, cardiovascular disease, and others who are at increased risk of developing kidney failure. The test is used to measure the level of waste product accumulated in your blood, called creatinine. A healthy kidney is capable of filtering up to 90ml/min. So, if the rate falls below that, you might be suffering from a kidney disease.
The doctor might also recommend a urine test, which helps evaluate the level of creatinine in your urine. In some cases, the doctor might recommend an ultrasound or an MRI to get a clear picture of the kidneys and detect any blockages. They might also conduct a biopsy where a small tissue from your kidney is extracted and checked under a microscope to determine the level of damage.
Treatment and Prevention of Kidney Disease
There’s no permanent cure for kidney disease, but a few steps can ensure your kidneys stay healthy.
- Manage your blood glucose levels if you are a diabetes patient
- Manage your blood pressure
- Do not take any medication that could worsen your kidney function
- Maintain your weight
- Follow a healthy lifestyle
- Avoid smoking
Conclusion
Kidney dialysis is an effective kidney disease treatment in Navi Mumbai. It’s recommended when you have reached the last stage of kidney disease and the last resort is to either get a kidney transplant or dialysis to save yourself. It removes excess waste from your body through a catheter. If that doesn’t work, your doctor might have to perform a kidney transplant to replace your kidney with the donor’s kidney.

Signs And Symptoms Of Asthma
Asthma is a lung disease and a chronic condition that requires ongoing medical treatment. Usually, when a person breathes, their airways are relaxed. However, in Asthma patients, the airway is narrow and blocked from mucus production. As a result, you might experience shortness of breath or difficulty breathing. You could also hear the whistling sound when breathing. A general physician in Navi Mumbai can diagnose Asthma based on your symptoms.
Asthma isn’t always a cause for concern for some people. It’s just a minor convenience, but for others, it can interfere with their daily life. Asthma attacks, especially, are life-threatening. Fortunately, medication can relieve these symptoms.
Types of Asthma
Asthma is categorized into different types based on the symptoms and complications. Here are the three types of Asthma:
- Intermittent: It doesn’t last long. Intermittent asthma goes away and comes back. It doesn’t persist.
- Persistent: Some patients are diagnosed with persistent asthma, which occurs often and the symptoms are more severe than intermittent asthma. The patient might also experience an asthma attack at times.
- Allergic: You can experience the symptoms of asthma when exposed to certain elements you are allergic to. This could be pet dander or mold.
Signs and Symptoms of Asthma
As mentioned earlier, the symptoms you experience depend on the type of asthma and what triggers it. Let’s check out a few common signs and symptoms of asthma:
- Chest pain
- Wheezing or whistling sound when you exhale
- Difficulty sleeping or staying asleep
- Coughing
- Shortness of breath
If the asthma worsens, you might experience these symptoms more often. You may have to use an inhaler. Asthma can be triggered by certain chemicals, gas, fumes, and dust.
Also Read: 5 Factors To Consider While Choosing A Right Multispecialty Hospital
Diagnosing Asthma
Your healthcare provider will ask about your family and medical history. You must tell them the history of any lung disease or existing allergies and respiratory disorders. They will order Spirometry, which measures airflow through your lungs to detect asthma. They might also order a blood test and chest X-ray to confirm the diagnosis.
Treatment for Asthma
Asthma can be treated with anti-inflammatory medication, which helps reduce inflammation in your airways, prevents mucus, and allows air to easily enter and exit the airways. You can take asthma medication orally, i.e. pills, or get an inhaler.
Although asthma is a chronic condition, it can be avoided if you know the trigger and stay away from it. For instance, if you are allergic to dust and dirt, make sure you work and stay in a clean, dust-free environment.
Identifying asthma symptoms early and taking quick action will prevent the condition from worsening. If you experience shortness of breath and it keeps getting worse, see a healthcare specialist immediately.
Conclusion
Asthma cannot be completely cured, but avoiding triggers and noticing the warning signs of an upcoming asthma attack can help you get quick relief. An asthma patient can go on to live a healthy and productive life given that they manage it well. Also, it’s important to check whether you have asthma or other respiratory disorders, which might produce similar symptoms.

How Stones Are Formed In Kidney?
Kidney stones, scientifically known as nephrolithiasis, are a common and painful urological condition. These small, solid, crystalline masses can form in the kidneys, causing immense discomfort and sometimes requiring medical intervention.
Let’s explore the formation of kidney stones, their causes, symptoms, and available treatment options. Here, you can also learn about the preventive measures, and the importance of seeking specialized care, such as Kidney Stone Treatment in Navi Mumbai at a leading healthcare facility for urological concerns.
What is a Kidney Stone?
Kidney stones are hard deposits in the kidneys when certain minerals and salts in the urine bind together. These stones can vary in size, from tiny particles resembling grains of sand to larger, more noticeable masses. Kidney stones can be composed of different substances, with calcium oxalate being the most common.
Causes of Kidney Stones
Understanding the formation of kidney stones begins with recognizing the factors that contribute to their development:
- A diet high in oxalate-rich foods like spinach, beets, nuts, and chocolate can increase the risk of kidney stone formation. Excessive consumption of sodium and animal protein can also be culprits.
- Inadequate fluid intake can lead to concentrated urine, making it easier for minerals to crystallize and form stones.
- Certain conditions like hyperparathyroidism and urinary tract infections can promote stone formation.
- Some medications, such as diuretics and antacids containing calcium, may contribute to kidney stone development.
Symptoms of Kidney Stones
The presence of kidney stones can result in a range of symptoms, including:
- Painful urination.
- Frequent urination in small amounts.
- Blood in the urine.
- Nausea and vomiting.
- Fever and chills.
- Severe pain in the back or side, often radiating to the lower abdomen and groin.
Also Read: Foods To Avoid With Kidney Stones
Treatment Options for Kidney Stones
When addressing kidney stones, prompt and appropriate treatment is essential. Kidney stone treatment at Mangal Prabhu Hospital in Navi Mumbai is offered by specialists who employ advanced techniques to manage this condition effectively.
a) Medication
Medication to relieve pain and facilitate stone passage may be prescribed for smaller stones that can be passed naturally.
b) Extracorporeal Shock Wave Lithotripsy
This non-invasive procedure uses shock waves to break down stones into smaller pieces, making them easier to pass.
c) Ureteroscopy
A thin tube with a camera is inserted into the urinary tract to locate and remove or break up stones.
Prevention of Kidney Stones
Taking steps to prevent kidney stones is crucial, especially if you have a history of stone formation or are at risk due to dietary choices or medical conditions:
- Stay well-hydrated by drinking plenty of water throughout the day to dilute urine and prevent mineral buildup.
- Limit high-oxalate foods, sodium, and animal protein consumption. Increase your intake of citrate-rich foods like citrus fruits.
- If you have a history of kidney stones, regular check-ups with a kidney stone specialist in Navi Mumbai can help monitor your condition and make necessary adjustments to your treatment plan.
Conclusion
Kidney stones are a painful and potentially recurrent condition that can significantly impact one’s quality of life. If you or a loved one is experiencing symptoms of kidney stones, seeking specialized care, like kidney stone treatment at Mangal Prabhu Hospital in Navi Mumbai, can make a significant difference in managing and preventing this condition. Remember that early intervention and preventive measures can help you enjoy a life free from the discomfort of kidney stones.
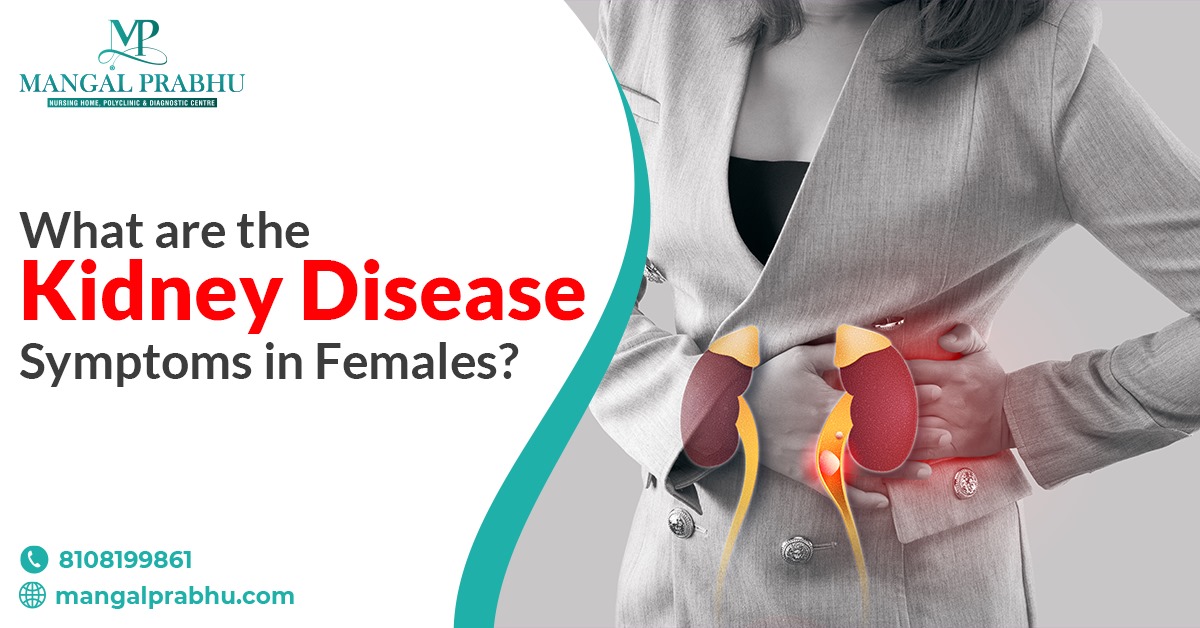
Can Hernia Be Treated Without Surgery?
A hernia is an unusual bulge caused by the organs that push through the weak muscle walls. The bulge is visible when you cough, sneeze, or put any kind of pressure on the affected area. Hernia can occur in the groin area, on your abdomen, and other parts of the body. They can be a birth defect or occur as you age. Hernias are also common in people who have undergone major surgery. Fortunately, hernia treatment in Navi Mumbai is available for those experiencing pain, discomfort, and other symptoms of hernia.
Non-Surgical Treatment Options
Unfortunately, the hernia will require surgery eventually. It doesn’t go away on its own. You can find temporary relief from certain medications, corsets that keep the bulge in place, and mild exercises, but these are only temporary solutions.
1) Medication:
Medication alone can’t help you get rid of a hernia, but it can relieve the symptoms and discomfort. For Hiatal hernia, you can take over-the-counter medication to relieve acid reflux and heartburn. Likewise, painkillers can help relieve pain.
2) Exercise:
If you practice high-intensity exercises or weightlifting, you might have to ask your healthcare provider if that’s safe. Any exercise that puts excess pressure on the bulge can make it worse. Talk to a hernia surgeon in Navi Mumbai and discuss the best exercises to prevent hernia from growing.
3) Dietary Changes:
Hiatal Hernias can cause GERD, heartburn, and many digestive issues. These are often triggered by certain foods that can cause your stomach acid to find its way to your throat. Take note of the foods that trigger these symptoms and focus on a healthy and balanced diet. Try to eat small and frequent meals.
4) Maintain a Healthy Weight:
Being overweight increases your risk of developing or worsening the existing hernia. It’s important to discuss your health goals with a healthcare provider and follow a weight-loss plan to shed those extra pounds.
Pros and Cons of Non-Surgical Treatments
As mentioned previously, hernia cannot be cured nor can it be reduced with manual treatments. You can take some steps to avoid the discomfort, pain, and other symptoms associated with the bulge, but you are eventually going to undergo surgery to have it fixed. The good news is a surgical procedure for hernia is minimally invasive and doesn’t take much time to heal.
You can also consider alternatives to open surgery, like robotic surgery or laparoscopic procedure. That said, not all types of hernias cause symptoms. There’s a chance the condition might go unnoticed and won’t require any repair either. It’s still best to consult your healthcare provider to ensure it won’t cause any complications. Let’s check out the pros and cons of non-surgical hernia treatments.
Advantages
- It can help reduce your hernia symptoms
- The non-invasive procedure doesn’t require any post-operative care
- You can carry out your routine activities
Disadvantages
- High risk of bowel obstruction
- Possibility of strangulation
- Hematoma
- Infections
See a healthcare specialist if you see the signs of hernia. Even if it’s causing any symptoms, it’s best to talk to a professional to rule out the possibility of any complications.

What Does A Pediatrician Do?
Pediatricians play a vital role in safeguarding the health and well-being of our most precious treasures – our children. These healthcare professionals specialize in the medical care of infants, children, and adolescents, addressing various medical issues specific to these age groups. Here, you can explore the essential role of a pediatrician, their responsibilities, and the importance of having a dedicated Children’s Hospital in Navi Mumbai for pediatric care.
Who is a Pediatrician?
A Pediatrician in Navi Mumbai is a medical doctor specializing in caring for children from birth to adolescence. Their primary focus is ensuring children grow and develop healthily and safely. Pediatricians are trained to diagnose and treat various medical conditions, provide preventive care, and guide parents and caregivers on child health and development.
What are the Responsibilities of a Pediatrician?
A pediatrician has these responsibilities regarding your child’s health, including:
1) Well-Baby and Well-Child Care
Pediatricians conduct routine check-ups to monitor a child’s growth, development, and overall health. These visits include vaccinations, physical examinations, and developmental assessments to ensure children meet important milestones.
2) Diagnosis and Treatment
When a child falls ill or experiences a medical issue, pediatricians are skilled in diagnosing the problem and providing appropriate treatment. It can range from common childhood illnesses like colds and flu to more complex conditions.
3) Preventive Care
Pediatricians emphasize preventive care through vaccinations, screenings, and counseling on nutrition, safety, and healthy lifestyle choices. Focusing on prevention, they help reduce children’s risk of illness and injury.
4) Chronic Disease Management
Some children may have chronic health conditions, such as asthma, diabetes, or allergies. Pediatricians work closely with families to manage these conditions and provide ongoing care and support.
5) Emergency Care
Pediatricians are often the first point of contact for parents in emergencies. They are trained to provide immediate care and stabilize a child’s condition before further treatment.
Also Read: What Is The Most Common Cause Of Premature Birth?
Why visit a Children’s Hospital?
Access to a dedicated Children’s Hospital in Navi Mumbai, like Mangal Prabhu Hospital, is crucial for pediatric care. Such hospitals are equipped with specialized facilities, equipment, and a team of well-versed healthcare professionals in pediatric medicine. Here’s why they are indispensable:
a) Child-Friendly Environment
Children’s hospitals are designed to create a welcoming and child-friendly atmosphere. It helps reduce anxiety and fear in young patients, making their healthcare experience more comfortable.
b) Specialized Pediatric Units
Children’s hospitals have specialized units and departments focused exclusively on pediatric care. It includes neonatal intensive care units (NICUs), pediatric intensive care units (PICUs), and pediatric surgery units.
c) Experienced Pediatric Specialists
Children’s hospitals have a team of pediatric specialists, including pediatric surgeons, pediatric neurologists, pediatric cardiologists, and more. These specialists are experts in diagnosing and treating specific childhood conditions.
Conclusion
Pediatricians are dedicated healthcare professionals who play a pivotal role in ensuring the health and well-being of children. They provide parents with essential medical care, preventive services, and guidance, helping children grow and thrive. A dedicated Children’s Hospital in Navi Mumbai, such as Mangal Prabhu Hospital, ensures that children receive the specialized care they need in a child-friendly and supportive environment. By collaborating with pediatricians and accessing specialized pediatric facilities, parents can rest assured that their children are in good hands regarding their healthcare needs.
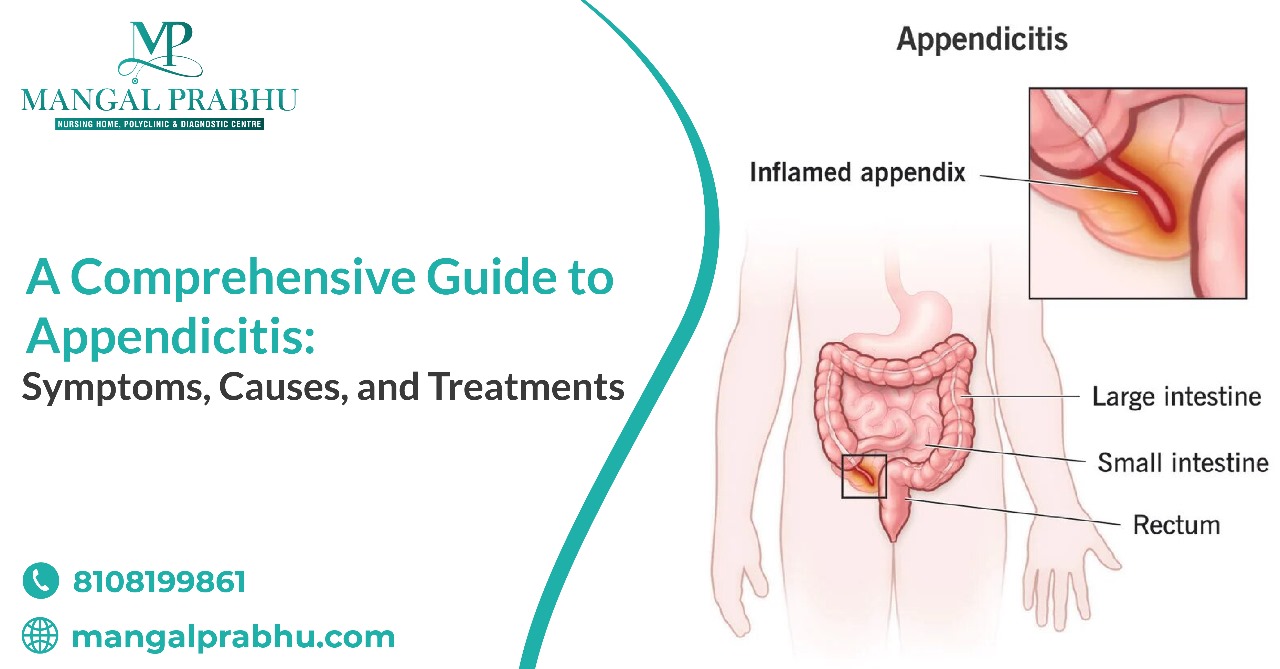
A Comprehensive Guide to Appendicitis: Symptoms, Causes, and Treatments
Introduction to Appendicitis
Appendicitis is a medical emergency when the appendix, a small, finger-like organ in the lower right side of the abdomen, becomes inflamed and infected. This condition can be extremely painful and, if left untreated, may lead to severe complications. This guide will explore the symptoms, causes, treatments, and prevention of appendicitis. If you’re in Navi Mumbai and require appendicitis treatment, it’s crucial to consult a skilled general surgeon in Navi Mumbai, such as those at Mangal Prabhu Hospital, who can provide timely and effective care.
Symptoms of Appendicitis
Recognizing the symptoms of appendicitis is essential for early diagnosis and prompt treatment. Common symptoms include:
i) Abdominal Pain
The most typical sign of appendicitis is a sharp pain that starts around the navel and gradually moves to the lower right abdomen. This pain often intensifies over time.
ii) Nausea and Vomiting
Many individuals with appendicitis experience nausea and may vomit due to the pain and discomfort.
iii) Loss of Appetite
A sudden loss of appetite is common when the appendix is inflamed.
iv) Fever
Appendicitis can lead to a low-grade fever, which may become more severe as the condition progresses.
v) Constipation or Diarrhea
Changes in bowel habits can occur, often with the patient experiencing either constipation or diarrhea.
vi) Abdominal Tenderness
The area around the appendix becomes tender and painful to the touch.
vii) Inability to Pass Gas
Some people with appendicitis find it difficult to pass gas.
Also Read: How To Reduce Appendix Pain?
Causes of Appendicitis
The exact cause of appendicitis is not always clear, but it is believed to result from one or more of the following factors:
a) Obstruction
Most cases of appendicitis are associated with a blockage in the appendix, often caused by stool, foreign objects, or an infection.
b) Infection
Infections within the digestive tract can lead to inflammation of the appendix.
c) Enlarged Lymphoid Follicles
Lymphoid tissue in the appendix can enlarge and lead to obstruction.
Treatments for Appendicitis
The standard treatment for appendicitis is surgical removal of the inflamed appendix, a procedure known as an appendectomy. This surgery can be performed using either traditional open or laparoscopic surgery, which is less invasive and typically results in a quicker recovery.
In some cases, if the appendix has formed an abscess (a pocket of infection), it may be drained before removing it surgically. It may involve a temporary drainage tube placement.
Prompt surgical intervention is crucial to prevent the appendix from rupturing, which can lead to severe complications, including peritonitis, a life-threatening infection of the abdominal lining.
Prevention of Appendicitis
- While appendicitis cannot always be prevented, some strategies may reduce the risk:
- Consuming a diet high in fiber may help prevent blockages in the appendix.
- Staying well-hydrated can help maintain healthy bowel function.
- Regular physical activity can promote overall digestive health.
- Practicing good hygiene, including regular handwashing, may reduce the risk of infection.
Conclusion
Appendicitis is a painful condition that requires prompt medical attention. You must consult a healthcare professional immediately if you experience symptoms like abdominal pain, nausea, vomiting, or fever. At Mangal Prabhu Hospital in Navi Mumbai, you can find experienced general surgeons who specialize in appendicitis treatment in Navi Mumbai. Early diagnosis and timely appendectomy are critical to a successful recovery and preventing complications. By understanding the symptoms, causes, and treatments of appendicitis, you can take the necessary steps to protect your health and well-being.

Is It Possible To Do Piles Treatment Without Surgery?
Piles can be a painful and uncomfortable condition affecting millions worldwide. Traditionally, surgical procedures have been the go-to option for treating piles. However, advancements in medical science have paved the way for non-surgical piles treatment options. Here, you will explore the possibilities of non-surgical treatment options. You’ll find this information valuable if you’re seeking Piles Treatment in Navi Mumbai.
What is Piles?
Piles, or hemorrhoids, are swollen blood vessels in the rectum or anus. They can be internal, occurring inside the rectum, or external, developing under the skin around the anus. Piles can be incredibly painful and lead to discomfort, bleeding, and itching. There are various causes behind the development of piles, making them a common health concern.
Causes and Symptoms of Piles
Several factors contribute to the development of piles, including chronic constipation, straining during bowel movements, pregnancy, obesity, and a sedentary lifestyle. Individuals with a family history of piles are also at an increased risk.
The symptoms of piles can vary from person to person, but common signs include:
- Rectal bleeding on toilet paper or in the toilet bowl after a bowel movement.
- Itching and irritation around the anus.
- Pain and discomfort during bowel movements.
- Swelling and lumps near the anus.
- Mucus discharge from the anus.
Non-Surgical Piles Treatment Options
Fortunately, surgery is not the only option for piles treatment. Non-surgical approaches have gained popularity due to their effectiveness and minimal invasiveness. Some of the non-surgical treatment options available include:
A) Medications
Over-the-counter creams and ointments can help relieve itching and pain associated with piles. A piles doctor in Navi Mumbai can prescribe prescription medication to reduce inflammation and discomfort.
B) Sclerotherapy
It involves injecting a chemical solution into the blood vessels around the piles, causing them to shrink and eventually disappear.
C) Rubber Band Ligation
In this procedure, a small rubber band is placed at the base of the pile, cutting off its blood supply. It causes the pile to shrink and fall off.
D) Infrared Coagulation (IRC)
IRC uses heat to shrink the blood vessels within the piles, reducing their size and relieving symptoms.
E) Laser Therapy
Laser treatment can precisely target and shrink piles, offering quick relief without surgery.
The Benefits of Non-Surgical Piles Treatment
Non-surgical piles treatment options offer several advantages over traditional surgical procedures:
- Minimal Pain
Non-surgical treatments are generally less painful, with shorter recovery times than surgery.
- Outpatient Procedures
Many non-surgical treatments can be performed on an outpatient basis, allowing patients to return home the same day.
- Lower Risk of Complications
Surgical procedures, such as infection and bleeding, carry certain risks. Non-surgical treatments have a lower risk of complications.
- Faster Recovery
Non-surgical treatments typically have quicker recovery times, allowing patients to resume their normal activities sooner.
Conclusion
Piles can be a source of immense discomfort, but it’s reassuring to know that surgery is not the only option for treatment. Non-surgical piles treatment options offer effective alternatives with fewer risks and a quicker recovery. If you’re in Navi Mumbai and seeking treatment for piles, consider consulting a piles doctor at Mangal Prabhu Hospital. At this hospital, you can explore various non-surgical options and find relief from this troublesome condition. Remember, early intervention and proper treatment can significantly improve your quality of life and prevent the condition from worsening.
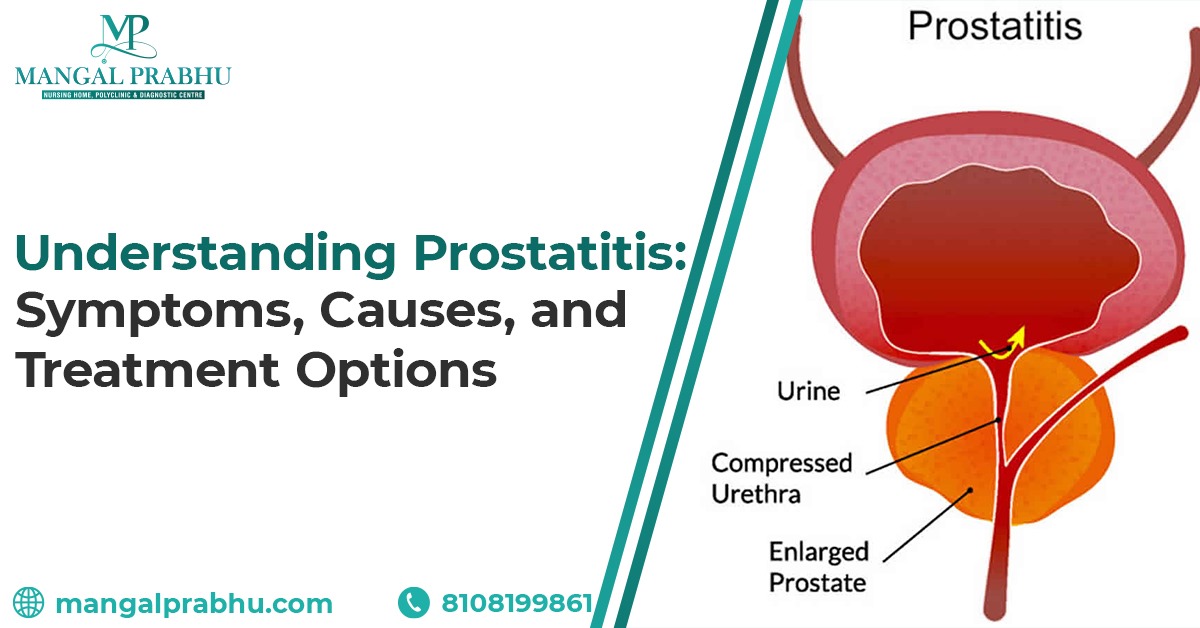
Understanding Prostatitis: Symptoms, Causes, and Treatment Options
Introduction to Prostatitis
Prostatitis is a common condition that affects many men. It refers to the inflammation of the prostate gland. The prostate gland is a small, walnut-sized organ located just below the bladder in men. It plays a crucial role in the reproductive system, producing semen that carries sperm. Prostatitis can cause various symptoms and discomfort. Hence, you should understand its symptoms, causes, and available treatment options. Here, you can learn about the available options for Prostate Infection Treatment in Navi Mumbai.
Symptoms of Prostatitis
Prostatitis can manifest in several ways. Its symptoms can range from mild to severe. Here are some common symptoms associated with prostatitis:
- Patients often experience pain in the lower abdomen. It can be sharp, dull, or throbbing in nature.
- Prostatitis can lead to urinary problems.
- Some men with prostatitis may notice sexual dysfunction.
- In some cases, prostatitis can cause flu-like symptoms.
Causes of Prostatitis
Prostatitis can have various causes, including bacterial infections, nonbacterial causes, and inflammatory conditions. Bacterial prostatitis occurs when bacteria infect the prostate gland, leading to inflammation. On the other hand, nonbacterial prostatitis can result from factors like autoimmune disorders or physical injury to the prostate.
Also Read: When Should I See A Urologist?
Treatment Options for Prostatitis
The treatment for prostatitis largely depends on its underlying cause and severity. Here are some common treatment options that Mangal Prabhu Hospital offers:
- Bacterial prostatitis is typically treated with antibiotics to eliminate the infection.
- For nonbacterial or chronic prostatitis cases, anti-inflammatory medications may help reduce inflammation and alleviate symptoms.
- Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage pain and discomfort associated with prostatitis.
- In some instances, alpha-blockers may be prescribed to relax the muscles in the prostate and bladder, improving urinary symptoms.
- Pelvic floor physical therapy can benefit individuals with chronic prostatitis by targeting muscle tension and improving pelvic floor function.
- Making lifestyle changes such as avoiding spicy foods, caffeine, and alcohol, as well as managing stress.
Prevention Tips for Prostatitis
While not all cases of prostatitis can be prevented, there are steps you can take to reduce your risk:
- Use condoms to reduce the risk of sexually transmitted infections that could lead to prostatitis.
- Drinking plenty of water can help maintain urinary tract health and reduce the risk of infection.
- Eating a balanced diet of fruits, vegetables, and whole grains can support prostate health.
- Staying physically active can help improve circulation and reduce the risk of prostate problems.
- Chronic stress can weaken the immune system, making the body more susceptible to infections. Practice stress-reduction techniques like meditation and yoga.
Conclusion
Prostatitis is a condition that can affect men of all ages, causing discomfort and disrupting daily life. If you experience prostatitis symptoms, seeking medical attention is essential. You can receive comprehensive care and specialized treatment for prostatitis and other urological conditions at Mangal Prabhu Hospital, a renowned healthcare facility with an expert Urologist in Navi Mumbai. Early diagnosis and appropriate treatment can help you manage prostatitis effectively and improve your quality of life. Remember to follow prevention tips and consult a healthcare professional for personalized guidance on prostate health.
Understanding Diabetes: Causes, Prevention, and How to Lead a Healthy Life
Introduction to Diabetes
Diabetes is a global health concern characterized by elevated blood sugar levels. It affects millions worldwide and can lead to severe health complications if not managed effectively. This article will explore diabetes, its causes, prevention strategies, and how to maintain a healthy life while living with this condition. See an experienced General Physician in Navi Mumbai who provides expert care if you find symptoms of diabetes.
Causes of Diabetes
Two main causes of diabetes are:
1) Genetics
Family history plays a significant role in determining an individual’s risk of developing diabetes. If you have close relatives with diabetes, your susceptibility to the condition may be higher. Genetic factors can predispose you to diabetes, making knowing your family’s medical history essential.
2) Lifestyle Factors
Unhealthy lifestyle choices contribute significantly to the risk of diabetes. A diet high in sugary and processed foods, a sedentary lifestyle with minimal physical activity, and chronic stress all increase the likelihood of developing diabetes. These factors can lead to weight gain, insulin resistance, and elevated blood sugar levels.
Prevention of Diabetes
Follow these methods to prevent diabetes, including:
a) Diet
Adopting a balanced and nutritious diet is essential in preventing diabetes. Emphasize whole grains, lean proteins, fruits, and vegetables in your meals. These foods help stabilize blood sugar levels and provide essential nutrients. Equally crucial is limiting the consumption of sugary and processed foods, which can lead to rapid spikes in blood sugar.
b) Exercise
Regular physical activity is a powerful tool in diabetes prevention. At least 150 minutes of moderate-intensity weekly exercise enhances insulin sensitivity and helps control blood sugar levels. Simple activities like brisk walking, cycling, or swimming can significantly reduce your risk of diabetes.
c) Supplements
Some supplements, such as chromium and cinnamon, have shown potential in controlling blood sugar. However, consulting with healthcare experts before incorporating supplements into your daily routine is essential. They can guide the safety and efficacy of these supplements based on your individual health needs.
Also Read: What Are Some Treatments For Hypertension?
Living with Diabetes
i) Managing Blood Sugar Levels
Regular monitoring of blood sugar levels is pivotal for effective diabetes management. Your healthcare team at Mangal Prabhu Hospital can guide you on when and how to check your blood sugar, helping you maintain optimal control.
ii) Healthy Lifestyle Habits
Beyond diet and exercise, a healthy lifestyle involves adequate sleep, stress management, and avoiding smoking and excessive alcohol consumption. These habits support overall well-being and contribute to better blood sugar control.
iii) Coping Strategies
Living with diabetes can be physically and emotionally challenging. Developing effective coping mechanisms is crucial for a fulfilling life. Seek support from healthcare professionals, friends, and family to help you navigate the challenges that may arise.
Conclusion
While diabetes is a chronic condition but manageable with the right knowledge and support, if you require diabetes treatment in Navi Mumbai, turn to Mangal Prabhu Hospital, a trusted healthcare partner dedicated to your well-being. Emphasize prevention through a healthy lifestyle, as early diagnosis and effective management are vital for individuals with diabetes. By making informed choices and seeking expert guidance, you can take control of your health.

How Long Does Chemo Take To Shrink A Tumor?
What is Chemotherapy, and How Does it Work
Chemotherapy is a medical treatment that uses powerful drugs to target and destroy cancer cells. It is a widely used approach in cancer treatment, either as a standalone therapy or combined with other treatments such as surgery or radiation therapy. Chemotherapy works by interfering with the growth and division of cancer cells, ultimately leading to their death. Visit an Oncologist in Navi Mumbai at Mangal Prabhu Hospital to learn more about chemotherapy treatment and its need.
Factors that Affect How Long Chemotherapy Takes
The duration it takes for chemotherapy to shrink a tumor can vary widely from person to person and depends on several factors:
i) Type of Tumor
The type of cancer and its aggressiveness play a significant role in determining how long chemotherapy will take to shrink a tumor. Some cancers respond more rapidly to chemotherapy than others.
ii) Size of Tumor
Larger tumors may require more time to respond to chemotherapy and show noticeable shrinkage. Smaller tumors may respond more quickly.
iii) Location of Tumor
The tumor’s location within the body can influence the time it takes for chemotherapy to have an effect. Tumors in easily accessible areas may respond more rapidly than those in challenging locations.
iv) Patient Health
A patient’s overall health and immune system strength can impact their response to chemotherapy. Patients in better health may tolerate and respond to treatment more effectively.
Treatment Options for Shrinking Tumors
Chemotherapy is just one of the treatment options available for shrinking tumors. The choice of treatment depends on the type and stage of cancer. Here are some common treatment options:
- Surgical removal of the tumor is often the first choice for solid tumors that are localized and haven’t spread. In some cases, surgery may be followed by chemotherapy to eliminate any remaining cancer cells.
- Radiation therapy uses high-energy rays to target and shrink tumors. Depending on the cancer type, it may be used with chemotherapy or as a standalone treatment.
- Immunotherapy enhances the body’s immune system to recognize and attack cancer cells. It has shown promising results in treating certain types of cancer.
Challenges Associated with Chemotherapy
While chemotherapy is a valuable tool in cancer treatment, it comes with challenges and potential side effects, including:
- Chemotherapy can cause various side effects.
- Some tumors may become resistant to chemotherapy over time, making it less effective.
- Chemotherapy is often administered in cycles, with rest periods in between. The overall duration of treatment can vary, ranging from a few weeks to several months or more.
Conclusion
The duration it takes for chemotherapy to shrink a tumor can vary based on several factors, including the type of tumor, its size, location, and the patient’s overall health. Chemotherapy is just one of the many treatment options available. Hence, you should choose the treatment after consulting with an oncologist specializing in cancer care.
At Mangal Prabhu Hospital, a leading Chemotherapy Center in Navi Mumbai, experienced oncologists work closely with patients to develop personalized treatment plans. Whether it’s chemotherapy, surgery, radiation therapy, or a combination of treatments, the goal is to provide the most effective and comprehensive care to combat cancer.