Advantages and Disadvantages of Removing Uterus
Hysterectomy or uterus removal is a major surgical procedure that’s performed in women with fibroids, uterine prolapse, cancer, and other reproductive issues. While the uterus removal surgery in Navi Mumbai can be a life-saving treatment for women, it comes with its share of drawbacks. Your gynecologist will discuss the advantages and disadvantages of removing the uterus to help you make an informed decision. Here’s what you should know.
Advantages of Removing the Uterus
1) Relief From Pain:
For women diagnosed with endometriosis, fibroids, and other uterine issues that cause heavy bleeding and significant pain during and in between the menstrual cycles, hysterectomy is the best possible treatment. It removes the source of these issues, improving your quality of life.
2) Prevent Recurring Fibroids:
Women with fibroids can have them removed while keeping the uterus intact. However, that comes with the risk of recurring fibroids. If you want permanent relief, hysterectomy is the most reliable option.
3) Reduced Risk of Uterine Cancer:
If you have a family history of uterine cancer, you may want to consider getting the uterus removed. That’s the only way to be assured that you won’t get uterine or endometrial cancer. In some cases, ovaries are also removed during the surgery, eliminating the risk of ovarian cancer.
Also Read: Which Surgery is Best for Uterus Removal?
Disadvantages of Removing the Uterus
i) Potential Hormonal Imbalances:
Uterus removal comes with significant hormonal changes, especially if the ovaries are removed. It induces immediate menopause in women, no matter how young they are. Menopause comes with hot flashes, mood swings, reduced bone density, and other symptoms that might be hard to cope with.
ii) Impact on Fertility:
The biggest drawback of hysterectomy is the loss of childbearing potential. Once you have had the surgery, you cannot become pregnant. This can result in a lifetime of regret for women of childbearing age.
iii) Possible Surgical Risks:
Like any major surgery, uterus removal requires an extensive hospital stay. Depending on where you get the surgery and the hospital’s protocol, you can expect to stay 1-3 days in the hospital post-surgery. Besides, it comes with the risk of surgical complications, like pulmonary embolism, hematoma, injury to nearby organs, and more.
Considerations Before Undergoing Surgery
A laparoscopic hysterectomy doctor in Navi Mumbai can perform a minimally invasive surgery, which involves a laparoscope that helps your surgeon remove the uterus without making a large incision on your abdomen. That said, it’s still advisable to consult a healthcare professional and discuss the recovery time and possible post-surgical complications before considering it.
Besides, you don’t necessarily need the uterus removal surgery. Alternatives like getting the fibroids removed (myomectomy), endometrial ablation, and medication can help relieve your symptoms. That said, the most viable treatment plan for you depends on your symptoms, their severity, and your fertility goals.
If you are past your childbearing age and are concerned about recurring fibroids, consider uterus removal. Talk to your gynecologist to figure out the best treatment option for your reproductive health issues. If you’ve decided on getting a hysterectomy, consider working with a gynecologist specializing in laparoscopic hysterectomy to minimize the risk of complications and ensure a faster recovery.

Is Normal Delivery Possible After Cervical Cerclage?
Cervical cerclage is done to prevent premature birth. Women who are at an increased risk of delivering a pre-term baby due to a weakened cervix might be offered this treatment. For women who are getting cervical cerclage, your biggest concern must be, “Is normal delivery possible after cervical cerclage”? Fortunately, yes. An obstetrician-gynecologist in Navi Mumbai might attempt normal delivery after removing cervical stitches. Here are more details about the procedure and the birthing options.
What is Cervical Cerclage?
Cervical cerclage refers to placing stitches on the cervix to keep it closed until you approach your delivery date. These will be removed when delivery is no longer considered premature. Your cervix is stitched when your doctor suspects a premature delivery because of an incompetent cervix, which is likely to open too soon, resulting in premature delivery.
The procedure is carried out around the second trimester and is mostly done on women with a history of pregnancy loss in the second trimester or a short cervix detected during an ultrasound.
Also Read : Most Common Cause of Vaginitis
Factors Influencing Delivery Method
Normal delivery is possible in women with a stitched cervix, although in a small percentage of cases, the healthcare provider recommends a c-section. Here’s what affects your delivery mode.
i) Cervix Health:
Your cervix needs to be intact and stabilized after cerclage removal if you want to attempt a vaginal delivery. Suppose the stitches weren’t removed already when you get into labor and the cervix tears. In that case, an immediate C-section delivery might be needed to prevent complications.
ii) Types of Cerclage:
Transvaginal cerclage, i.e., placing the stitches through the vagina, is the most common method of cerclage. Vaginal delivery is likely after transvaginal cerclage, as these can be removed before labor. Transabdominal cerclage, however, is a more complex procedure that involves stitching the cervix through your abdomen. In a transabdominal cerclage, the stitches remain in place, requiring a cesarean delivery.
iii) How Labor Progresses:
If labor progresses well and there’s no sign of an infection, fetal distress, or other complications, there’s a good chance you’ll deliver vaginally. If you experience pre-term labor, a c-section might be a safer bet.
Normal Delivery After Cervical Cerclage
You can talk to your doctor about a suitable time for a cervical cerclage removal surgery in Navi Mumbai to prepare yourself for vaginal birth. Once the stitches are removed and your cervix appears functional, you can opt for a normal delivery.
Potential Risks and Challenges
If the cervix is unable to maintain stability or strength for labor post-cerclage removal, cesarean delivery may be more appropriate. That’s because labor can cause cervical tears. There’s also a risk of infection around the surgical site, which can lead to complications during labor. Moreover, your doctor will remove cervical stitches around the 36th week of gestation, which might increase the chances of pre-term labor and birth. Vaginal delivery isn’t possible in cases with a history of multiple c-section deliveries. Your doctor will explain the risks and benefits of each delivery method, helping you make an informed decision.
What are the 1st Signs of Menopause?
Menopause is a significant natural change that occurs in a woman’s life in her 40s and 50s. It marks the end of your fertility journey. Once you’ve entered menopause, you will stop having periods. Your ovaries will stop producing estrogen and progesterone — the two vital hormones responsible for your fertility. Menopause happens gradually.
The symptoms can, however, be physically and mentally overwhelming. Knowing what to expect can prepare you for hot flashes, mood swings, and other menopausal symptoms. So, what are the 1st signs of menopause? And when should you see a gynecologist in Navi Mumbai? Let’s find out.
Common Early Symptoms of Menopause
1) Irregular Menstrual Cycles:
The earliest and most obvious sign of menopause is irregular periods. You may have a menstrual cycle one month and skip the next month, or you may go months without periods. The fluctuating period is the biggest sign that menopause is approaching. If there’s a two-month gap between your menstrual cycles, you could already be in your perimenopause. The flow could be heavier or lighter.
2) Hot Flashes:
The sudden onset of hot flashes, which may happen at unexpected times and last a minute or longer, is another early sign of menopause. Night sweats might become more common, and you’ll notice a rapid heartbeat with intense warmth.
3) Emotional Changes:
Menopause can put you on an emotional rollercoaster. One minute, you are happy, and before you know it, you’ll feel sad, anxious, and depressed. A drastic drop in estrogen accompanied by disrupted sleep can be the cause.
Physical Changes
a) Weight Changes:
Low estrogen can shift the fat stored in your thighs and hips to the abdomen. It also affects your metabolism, making it difficult for your body to burn fat. Besides, women in their 40s and 50s tend to exercise less, making weight management difficult.
b) Hair Loss:
Estrogen is again blamed for hair thinning and loss during menopause. Dropped estrogen makes testosterone dominant, which can cause a receding hairline. This male hormone is also responsible for unwanted hair growth on the face, like the chin and upper lip.
Sleep Disruptions
Menopause can disrupt your sleep cycle. Some women sweat a lot at night and might wake up drenched, which can affect their sleep. Other women are unable to fall asleep at all or might wake up frequently throughout the night.
Cognitive and Emotional Effects
Menopause is an emotionally tough time. You experience one of the biggest transitions, from your childbearing age to a new midlife. This can make mood swings frequent. The mood swings can sometimes be so severe that they can turn into depression.
Brain fog is another common symptom that women nearing menopause report. If you’ve been having a hard time concentrating or remembering things, it could be an early sign of menopause.
Importance of Medical Consultation
Whether or not you need menopause treatment in Navi Mumbai depends on the severity of your symptoms. Some women don’t even notice the changes, while others go into depression. If you feel hopeless, helpless, or have lost interest in all activities, consult a gynecologist.

Most Common Cause of Vaginitis
Most women experience itching, discomfort, swelling, an unusual discharge, and pain down there at some point. These often indicate vaginitis. The most common cause of vaginitis is bacterial infection, but yeast infection and certain sexually transmitted infections can also be the culprits. If you notice the above symptoms and feel any unusual change in your vaginal health, visit an obstetrician-gynecologist in Navi Mumbai to diagnose the underlying cause. In the meantime,
let’s explore the most common cause of vaginitis.
i) Bacterial Vaginosis
There’s usually a mix of good and bad bacteria, with good bacteria keeping the vaginal environment slightly acidic. Bacterial Vaginosis (BV) occurs when there’s an increased amount of bad bacteria in your vagina.
a) BV Causes:
BV can be linked to douching and using scented products, which can affect the pH balance of your vagina. It’s also more common in women with multiple sexual partners, as it increases the risk of bacteria entering your vagina.
b) BV Symptoms:
If there’s an overgrowth of the bad bacteria, you might develop bacterial vaginosis, causing grayish discharge, a fishy odor, vaginal itching, and discomfort.
c) BV Treatment:
Treatment includes an antibiotic course. Make sure you take the pills even if the symptoms improve, as there’s a risk of recurrence.
ii) Yeast Infections
The overgrowth of Candida albicans — a fungus that naturally thrives in your vagina — can cause vaginitis. It’s also found in other moist areas of your body and is also a common reason for diaper rash in babies.
d) Yeast Infection Causes:
Yeast infection occurs because of hormonal changes and increased blood glucose levels in people who are taking antibiotics. Antibiotics kill good bacteria, which are responsible for keeping Candida albicans in check.
e) Yeast Infection Symptoms:
Symptoms include itching and redness around the vulva with thick discharge.
f) Yeast Infection Treatment:
Antifungal creams and oral medication can help clear yeast infections. You can also take probiotic supplements to restore a healthy balance of good and bad bacteria. Lifestyle changes, like avoiding damp and tight clothing, can also help.
iii) Trichomoniasis
Trichomonas vaginalis is transmitted through sexual intercourse with an infected partner. The infection affects the urinary tract system in men and the vagina in women.
g) Trichomoniasis Symptoms:
Symptoms may vary from woman to woman, but most infected people experience itching, greenish-yellow discharge, and pain during urination and intercourse.
h) Trichomoniasis Treatment:
Oral antibiotics can help clear Trichomoniasis. Avoid sexual activity until it’s completely cleared.
iv) Other Less Common Causes
Vaginitis is also linked to causes other than bacteria, parasitic, and fungal infections. Let’s discuss a few less common yet possible causes:
i) Allergic Reaction:
Scented products, such as soaps and creams, can cause an allergic reaction or may simply irritate your vagina, causing a burning sensation and redness. The sensitive skin of your vagina can also become swollen and red from the laundry detergents and condoms.
j) Vaginal Atrophy:
Women approaching menopause or post-menopausal women are at increased risk of vaginal atrophy due to a decreased production of estrogen. Your vaginal walls become thin and dry without estrogen, increasing the risk of vaginitis. Your gynecologist will run tests to diagnose the cause and offer the most appropriate vaginitis treatment in Navi Mumbai. See your doctor if you notice the above symptoms. Stay healthy!!

What Causes Lower Abdominal Pain in Females?
Cramping or lower abdominal pain is not uncommon in women. When you reach puberty and menstruation begins, you are likely to have dull or sharp pain in the lower abdomen — the area between your belly button and groin. It’s also referred to as pelvic pain. Lower abdominal pain in women can indicate many issues.
Some are normal and just a part of your menstrual and ovulation cycle. There’s a possibility that pelvic can be due to a serious underlying condition, especially if it’s persistent and is accompanied by other unusual symptoms. It’s best to see a gynecologist in Navi Mumbai to rule out any life-threatening condition. Let’s check out some common causes of pelvic or lower abdominal pain in females.
Menstrual Cramps
Menstruation is the most common cause of pelvic pain in women. It may feel like sharp pain in your upper and lower abdomen and can even spread to the lower back in some cases. The pain is manageable with over-the-counter painkillers and a hot water pad. Menstrual cramps begin before your period starts, as your uterus starts contracting. It can last 2-3 days.
Ovulation Pain
The German word ‘mittelschmerz’ is used to define painful ovulation. In the middle of your menstrual cycle, your ovary releases an egg and fluid. The egg goes down your fallopian tubes into the uterus. The fluid can sometimes enter your abdomen, which may cause irritation and pain. Ovulation pain is temporary and occurs on one side of the pelvis.
Urinary Tract Infections (UTIs)
Lower abdominal pain with painful urination can indicate UTI. Urinary tract infections occur when bacteria from the vagina, skin, or rectal area travel up the urethra into the bladder and occasionally reach the kidneys. UTI can occur in any part of the women’s urinary tract.
Gastrointestinal Issues
Lower abdominal pain could simply be the wind trapped in your abdomen or a sign of constipation. Irritable Bowel Syndrome (IBS) can also cause pelvic pain. If the pain persists and is accompanied by constipation, diarrhea, and other symptoms, it’s advisable to discuss abdominal pain treatment in Navi Mumbai with a certified physician.
Reproductive Health Concerns
Pelvic pain can indicate reproductive health concerns in women. Examples include endometriosis — a condition in which the tissue similar to your uterine lining grows outside the uterus and shed during your period. This can cause excessive bleeding with chronic pelvic pain.
Pelvic Inflammatory Disease (PID) is an infection in the reproductive organs from an untreated sexually transmitted disease. Lower abdominal pain with fever and unusual vaginal discharge are the common symptoms of PID.
Both medical issues can affect your fertility.
When to See a Doctor
- Sharp pain in the lower right abdomen that gets worse over time. It can indicate appendicitis, which can be a medical emergency.
- Persistent pain with fever, chills, and heavy bleeding.
- You suspect an infection that could be causing the pain.
Pelvic pain isn’t always severe or requires a visit to a gynecologist. However, if you notice the above symptoms, seek immediate medical care.
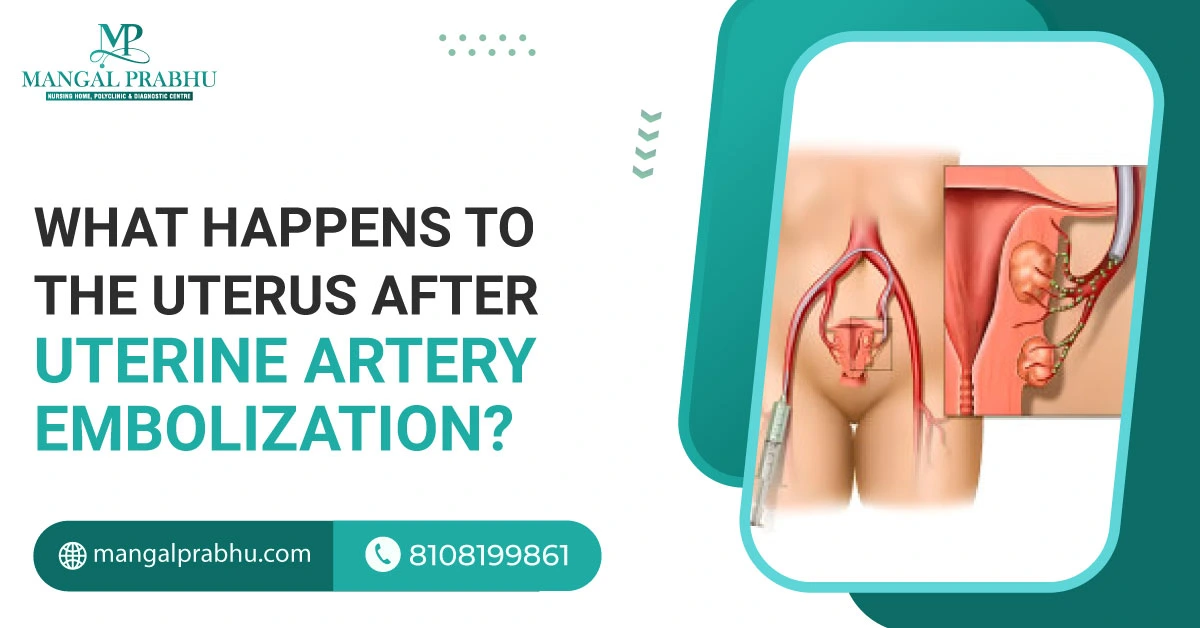
What Happens to the Uterus After Uterine Artery Embolization?
Women experiencing heavy bleeding due to uterine fibroids, malignant growth, and other medical conditions can opt for Uterine Artery Embolization treatment in Navi Mumbai. It’s a less-invasive alternative to open uterus surgery for removing fibroids and the uterus. The procedure cuts the blood supply to the fibroids, making them shrink and eventually die. This is also an effective way to control excessive bleeding. The question is, what happens to the uterus after uterine artery embolization? Let’s find out.
Immediate Aftereffects
You will be given sedatives and medication that numbs your groin area. So, you won’t feel a thing during the procedure. You are supposed to lie straight for 5-6 hours. Afterward, when the effect of the anesthesia wears off, you might experience mild cramping and some discomfort. Your doctor will prescribe pain medication. The pelvic pain can be moderate or severe for the first few days following the UAE.
Short-term Changes
The major goal of the procedure is to reduce the fibroid size and control heavy bleeding. Here’s what you can expect during recovery:
a) Reduction in the Fibroid Size:
After the procedure, the blood supply to the fibroid is cut off, and their size will gradually decrease. It may take weeks or months for them to die, though. If the fibroids are located close to the uterine lining, they might expel through your vagina. You can expect some bleeding if that happens.
b) Pelvic Pain Relief:
Once the fibroids die, you will notice an improvement in your pelvic pain. Women with urinary incontinence due to fibroids putting pressure on the bladder will also notice improvement in their symptoms.
c) Regulate Menstrual Cycles:
After UAE, you may notice slight bleeding and skip periods for a few weeks. Your periods will gradually return, initially with light bleeding and then regular menstrual bleeding. This will be better and comparatively lighter than the pre-procedure state.
Long-term Outcomes
Although the procedure’s outcome is great, with patients reporting no heavy bleeding after UAE, it does come with its share of risks.
A) Fertility Issues:
It’s possible to get pregnant after UAE, but it comes with an increased risk of miscarriage and preterm birth. It’s best to talk about the potential complications with your gynecologist.
B) Additional Treatment:
UAE is very effective, but there’s a chance the fibroids will return or the existing ones will not die completely. If the treatment doesn’t work, you may need to consider surgery for fibroid removal or hysterectomy.
When to See Your Doctor?
Pelvic pain is not uncommon after the UAE. It can start in 24 hours and may last a few days. You can take over-the-counter painkillers to relieve pelvic discomfort. However, if the pain persists or is too severe to let you perform routine tasks or work, report it to your doctor. Other unusual symptoms after UAE are a high-grade fever with a vaginal discharge (this might indicate an infection) and heavy bleeding.
Conclusion
The process is safe overall, but it’s better to stay in touch with your gynecologist and watch for the warning signs mentioned above. Once you’ve had uterine artery embolization, it’s only a matter of time before you can resume your work like usual.
Sleeping Position After D&C
Dilatation and curettage (D&C) treatment in Navi Mumbai is a minimally invasive surgical procedure in which the doctor uses medicine or tools to open your cervix and insert instruments that scrape the uterine surface. This removes the uterine tissues. A suction can also be used for the procedure.
Although there’s no specific sleep position for a D&C patient, some positions can help you get good quality sleep. Below, we’ve discussed the best sleeping position after D&C.
Recommended Sleeping Positions
a) Sleeping On Your Back
This is the most comfortable position for a woman who has just gone through D&C. It doesn’t put pressure on your abdomen, allowing your body, especially the pelvic region, to heal after surgery. It also provides relief from cramping and discomfort. Sleeping on your back is also good for blood circulation. The better your blood circulation, the faster you will heal.
b) Sleeping On Your Side
Another doctor-recommended sleep position after D&C is on your side. Side sleeping (left and right) is considered safe and a good option for women experiencing mild cramping, bloating, and back pain. It also promotes good blood flow, which supplies nutrients to the healing tissues, speeding up your recovery.
Positions to Avoid
A) Sleeping On Your Stomach
Gynecologists in Navi Mumbai do not recommend this position, as it puts unnecessary strain on your abdomen and pelvis. As your uterus contracts and goes back to its normal size, it may cause cramps. To relieve the pain, it’s advisable to sleep in a position that feels relaxing.
B) Sleeping in a Curled-up Position
While it may feel comfortable to get curled up like a fetus in a mother’s womb, it’s not a safe position after D&C. It brings your knees close to your chest, which may strain your abdominal and pelvic muscles. It can make your cramping worse and increase discomfort. Besides, this sleep position has many side effects, like joint stiffness, muscle ache, difficulty breathing, back strain, and so on.
Tips for Comfort
1) Using Supportive Pillows
Consider adding a pillow under your knee and the back to prevent back strain and abdominal pain after surgery. You can also hug a pillow to get chest support. Pillows under your legs will keep your spine in the most comfortable position while you sleep.
2) Maintaining the Right Environment
In addition to the sleep position, the sleep environment matters. Turn off your phone, remove distractions, turn off the lights, and keep the room’s temperature comfortable. Creating a cozy environment will help you fall and stay asleep.
3) Listen to Your Body
If you feel pain or your symptoms get worse in any sleeping position, switch immediately.
Conclusion
D&C is mainly performed on women who want an abortion or suffer a miscarriage. The procedure can also be used for testing. It can detect uterine fibroids, polyps, and other uterine-related issues that cause abnormal bleeding, pelvic pain, and other unusual symptoms. It’s a relatively safe procedure, but a good sleep position with a balanced diet and a proper exercise routine is crucial for quick recovery.

Which Surgery is Best for Uterus Removal?
Hysterectomy is the surgical removal of the woman’s uterus. It’s often considered a last resort for medical issues like endometriosis, uterine fibroids, polyps, cancer, enlarged uterus, uterine prolapse, and uterine rupture. The surgery, however, comes with potential risks. A woman can’t get pregnant without a uterus.
Moreover, if your ovaries were removed during hysterectomy, you will enter menopause immediately. Choose the best hysterectomy surgeon in Navi Mumbai and understand the different surgical methods used for hysterectomy.
Types of Uterus Removal Surgeries
1) Abdominal Hysterectomy
An open abdominal surgery is common for uterine fibroids, hyperplasia, and certain types of cancer. The surgeon makes a 5-7-inch cut either vertically or horizontally above your pubic bone and removes the uterus. If required, the doctor might perform an immediate oophorectomy (ovaries removal) and salpingectomy (fallopian tube removal).
Pros:
- It gives your surgeon a direct access to the uterus and a clear view of the surrounding organs.
- It’s effective for certain conditions where less-invasive procedures might not work.
- The doctor can easily detect any abnormality in your ovaries, fallopian tubes, cervix, and other reproductive parts during the surgery
Cons:
- Longer hospital stay
- Slow recovery
- Higher risk of post-surgical complications
- Scarring
2) Vaginal Hysterectomy
Vaginal hysterectomy is the least invasive and most preferred option for women undergoing hysterectomy. The surgeon makes a small incision on the top of your vagina and uses special instruments to detach the uterus and remove it through the vagina.
Pros:
- It’s performed on an outpatient basis, which means the patient can go home within 24 hours after the procedure.
- Fewer complications
- Quick recovery
- No scarring
Cons:
- It can lead to incomplete removal of the uterine tissues
- Infection around the incision
3) Laparoscopic Hysterectomy
A laparoscope is a thin tube with light and a camera attached to its end. A uterus removal surgery in Navi Mumbai is mainly performed with a laparoscope. The surgeon administers local anesthesia and makes small incisions on your abdomen (about half an inch). They insert a laparoscope into one of the holes, cut the uterus into small pieces, and remove it through the vagina.
Pros:
- Faster healing and quick recovery
- Fewer complications
- Shorter hospital stay
- Lower risk of infection
Cons:
- Not effective for patients with large uterine fibroids, hyperplasia, malignant tumors, and advanced endometriosis.
4) Robotic-assisted Hysterectomy
Robot-assisted hysterectomy is similar to a laparoscopic procedure. The only difference is that a robotic arm is used to perform a hysterectomy.
Pros:
- Offer greater precision
- Short hospital stay
- Fast recovery
Cons:
- Not effective for all cases
Factors to Consider When Choosing a Surgery
A vaginal hysterectomy is the best option for women who want to recover faster and get back to work within 2-3 weeks. There are fewer to no complications, and you can go home the same day after surgery. Laparoscopic hysterectomy is the second-best option. If vaginal hysterectomy is not possible due to an enlarged uterus or fibroids, or other serious issues, your doctor will advise laparoscopic hysterectomy.
The surgeon will consider the patient’s age, health status, uterus size, and previous scars when advising the hysterectomy surgery method.

What is The Best Treatment for Pelvic Inflammatory Disease?
PID stands for Pelvic Inflammatory Diseases which is a severe type of infection that occurs to the organs found in the female reproductive system such as the uterus, fallopian tubes, and other similar ‘organs’. It is an inflammation of the reproductive tract commonly attributed to some infections getting into the tract especially sexually transmitted infections (STIs).
Specifically, PID being a severe condition that if not well treated on time leads to many other severe health problems on women. This post looks at the different methods that can be used in the treatment of PID and in essence emphasizes on the need to prevent the infection through practicing safe sex and having regular checkups with a gynaecologist.
Common treatment options for PID
A. Antibiotic Therapy
Antibiotic treatment is the widely recommended as well as the most efficient treatment of PID. This disease can be thoroughly managed through the prescription of antibiotics which is known to be the most effective treatment strategy. Antibiotics are drugs that help the body to fight against the conditions that cause PID.
Different antibiotics need distinct time and normally doctors give a pack of many antibiotics for two weeks to be completely effective in eradicating all bacteria. In majority of cases, proper courses of antibiotic treatment are needed, which is possible only with the help of a gynaecologist in Navi Mumbai.
As much as is needed, it is extremely crucial to stick to the complete often-prescribed course of antibiotic treatment.
B. Pain Management
In relation to the management of PID, pain killing is also a powerful tool that is used in the treatment process in conjunction with antibiotics. Nonsteroidal anti-inflammatory drugs or NSAIDs such as Ibuprofen may be prescribed to the patient in order to reduce inflammations while mild pain relievers may be used in case of mild pains and casual pains may be prescribed by a doctor as a prescription pain medicines.. Applying a hot water bag or hot fomentation on the lower abdomen sometimes offers comfort. A gynaecologist in Navi Mumbai can help assess the pain and suggest the right pain management approach.
Exploring alternative treatments for PID
A. Herbal remedies
Certain herbal remedies are sometimes used as a complementary treatment for PID. However, medical research evidence supporting their efficacy is still limited. Some herbs believed to possess antimicrobial properties and traditionally used for gynaecological issues are garlic, turmeric, and neem. However, combining herbal remedies with prescribed antibiotic treatment is best under a doctor’s guidance.
B. Physical therapy
Strengthening exercises such as gentle pelvic floor and abdominal exercises permitted by a physical therapist can alleviate the pain and soreness of muscular tissues caused by PID. Then, balanced and low-impact exercises such as walking and swimming can be resumed during the later phase of recovery. These should not, however, be used in place of medical treatment. It is most effective when used with medication by a gynaecologist in Navi Mumbai concerning antibiotics and painkillers.
Conclusion
while antibiotic therapy remains the primary treatment modality for PID, it is equally important to manage the associated pain and consider complementary therapies safely. However, prevention of STIs through safe sex and early screening during Pelvic Inflammatory Disease Treatment in Navi Mumbai is critical to avoiding PID and its potentially severe repercussions on reproductive health in the long run. Prompt guidance from an experienced gynaecologist is advisable for early PID diagnosis and most effective patient care plan suited to individual needs.

Symptoms of PCOD Problem in Females
Polycystic Ovarian Syndrome, or PCOD, occurs in women during their reproductive age. It disturbs the production of the woman’s reproductive hormones, estrogen and progesterone. Fortunately, PCOD treatment in Navi Mumbai is available for those experiencing the painful symptoms.
PCOD causes irregular periods, as the mature eggs that are supposed to be released from your ovaries once a month might not mature or get released. PCOD also occurs when there’s excess production of male hormone androgen in the woman’s reproductive system.
Symptoms of PCOD problem in females
You might notice the symptoms of PCOD when your menstruation starts, but symptoms can also show up later, i.e., in your 20s and 30s. Here are some common symptoms of Polycystic Ovarian Syndrome.
1) Irregular Periods:
The most common symptom of PCOD is irregular periods. The regular menstruation cycle is 28 days. However, if you have PCOD, you might notice your period getting delayed by ten or more days. Some women experience periods that last longer than nine days and occur frequently.
2) Infertility:
Difficulty conceiving is another symptom of PCOD. Since your periods and ovulation cycle are irregular, you might have difficulty getting pregnant.
3) Excess Androgen:
Women’s reproductive organs produce a small amount of androgen. However, those with PCOD report excess androgen production, which can lead to excessive hair fall, excess hair on the face and body, and acne.
In addition to these, PCOD can result in rapid weight gain.
Also Read: PCOD vs PCOS: Difference Between PCOD and PCOS
Causes of PCOD
The exact cause of PCOD is unknown, but the following conditions can increase your risk of developing this hormonal disorder.
i) Insulin Resistance:
If your body produces too much insulin, the level of androgen might also rise significantly, and this will affect the ability of your ovaries to release mature eggs.
ii) Heredity:
People with a family history of PCOD might develop this condition in their reproductive years. Certain genes are linked to PCOD.
Risks and Complications of Untreated PCOD
PCOD can affect your fertility. It increases the risk of inability to conceive, miscarriage, and premature birth. In pregnant women, untreated PCOD can lead to gestational diabetes and hypertension. Moreover, it can cause mental health issues, such as depression and anxiety, which are often linked to excessive weight and hair loss.
Diagnosis of PCOD
A gynecologist in Navi Mumbai will ask you about the symptoms and menstrual cycle and take a physical exam to diagnose PCOD. An ultrasound can help confirm the presence of ovarian cysts. They also recommend a blood test to check your insulin level and the overall hormonal balance.
Treatment Options for PCOD
There’s no permanent cure for PCOD, although symptoms can be managed with a balanced diet and a healthy lifestyle. Your gynecologist will prescribe medication for excessive hair growth on your body, hair loss, acne, sleep apnea, and irregular menstrual cycle. For fertility issues, a surgical procedure that removes ovarian cysts and destroys male-hormone-producing tissues can help.
Conclusion
Getting pregnant with PCOD is possible, but the condition requires treatment. Managing the symptoms, such as excessive weight and irregular periods, can help improve your quality of life and your reproductive health.